Feasibility of normal tissue dose reduction in radiotherapy using low strength magnetic field
Article information
Abstract
Purpose
Toxicity of mucosa is one of the major concerns of radiotherapy (RT), when a target tumor is located near a mucosal lined organ. Energy of photon RT is transferred primarily by secondary electrons. If these secondary electrons could be removed in an internal cavity of mucosal lined organ, the mucosa will be spared without compromising the target tumor dose. The purpose of this study was to present a RT dose reduction in near target inner-surface (NTIS) of internal cavity, using Lorentz force of magnetic field.
Materials and Methods
Tissue equivalent phantoms, composed with a cylinder shaped internal cavity, and adjacent a target tumor part, were developed. The phantoms were irradiated using 6 MV photon beam, with or without 0.3 T of perpendicular magnetic field. Two experimental models were developed: single beam model (SBM) to analyze central axis dose distributions and multiple beam model (MBM) to simulate a clinical case of prostate cancer with rectum. RT dose of NTIS of internal cavity and target tumor area (TTA) were measured.
Results
With magnetic field applied, bending effect of dose distribution was visualized. The depth dose distribution of SBM showed 28.1% dose reduction of NTIS and little difference in dose of TTA with magnetic field. In MBM, cross-sectional dose of NTIS was reduced by 33.1% with magnetic field, while TTA dose were the same, irrespective of magnetic field.
Conclusion
RT dose of mucosal lined organ, located near treatment target, could be modulated by perpendicular magnetic field.
Introduction
Increase target tumor dose without significant complications is a primary goal of radiotherapy (RT). Mucosal lined organs (gastrointestinal tract and airway) have low radiation tolerance [123], and its complications are one of major obstacles of RT. When a mucosal lined organ located near a target tumor, even with advanced modern RT techniques, it is difficult to deliver sufficient dose to the target tumor [45].
In photon RT, interaction between incident high energy photons and body tissue's electrons produce secondary electrons. Chemical reactions induced by these secondary electrons are known as major molecular mechanism of RT. Due to kinetic energy transmitted from the photon, deposition of the secondary electron is occurred after travel a few millimeters in the forward direction from the interaction point. Because there are no interaction points upstream from the surface to produce secondary electrons, RT dose of the surface dose is low. This phenomenon that body surface gets significantly lower dose in photon RT, is known as 'build up phenomenon' or 'skin sparing effect.'
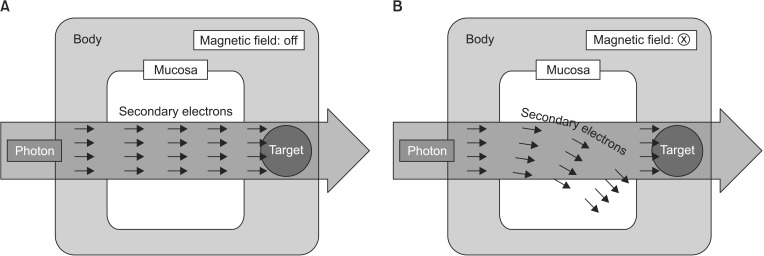
When photon RT is given to a target tumor near a mucosal lined organ, near target portion of inner-surface (NTIS, i.e., mucosa) is damaged by secondary electrons which produced in upstream body tissue. If those secondary electrons removed before deposit in NTIS, NTIS would not get high RT dose, then NTIS could be spared. On the other hand, new secondary electrons produced in NTIS, would be transferred to the target tumor, so the target tumor's RT dose might be preserved.
This hypothetic phenomenon could be possible, when electrons are selectively removed in an internal cavity of the mucosal lined organ, while photons are not affected. Magnetic field, which does not interact with photons, but interact with electrons, could be utilized for this purpose. The aim of this study is to demonstrate RT dose reduction in NTIS of internal cavity (i.e., mucosa of the mucosal lined organ) using low strength magnetic field, with phantom model experiments.
Materials and Methods
1. Target tumor and mucosal lined organ
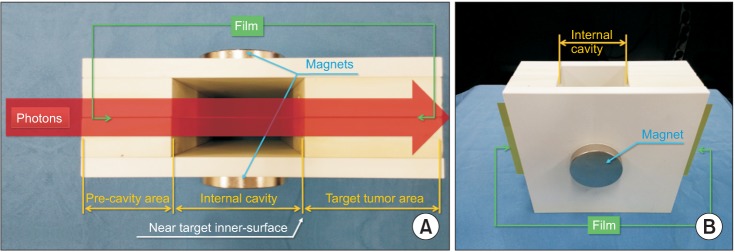
A phantom model in which a target tumor area (TTA) is located near an internal cavity was developed (Fig. 1). While photon radiation passed through both the internal cavity and the target tumor, magnetic field was applied to the phantom. Dose distributions were analyzed through beam path, including the internal cavity and the TTA.
2. Single beam model experiment
First experimental model was single beam model (SBM) by which longitudinal depth dose distribution was measured. Tissue equivalent (density, 1.045 g/cm3) polystyrene based phantom, composed of air filled internal cavity and TTA, was made (Fig. 2). Magnetic field of 0.3 T was applied in perpendicular direction to radiation beam path. The magnetic field was generated by two 5 cm × 5 cm sized neodymium magnets located both side of the phantom. Radiochromic film (GafChromic EBT3; International Specialty Products, Wayne, NJ, USA) was positioned longitudinal direction to radiation beam path to measure central axis absorbed dose. Six MV photon beam of 3 cm × 3 cm field size was delivered to the SBM phantom with or without magnetic field applied. Prescribed RT dose of TTA was 900 cGy.
3. Multiple beam model experiment
Multiple beam model (MBM) simulated a clinical case of prostate cancer in which rectum (mucosal lined organ) is close to the target tumor (Fig. 3). MBM phantom was composed of a round cylinder shaped internal cavity which had 4 cm inner-diameter and TTA. Cross-sectional absorbed dose was measured at two separate points: 1) inner-surface of the internal cavity (including NTIS) and 2) TTA. The distance between NTIS and TTA was 5 mm. The phantom was irradiated with 3 different beam fields as shown in Fig. 3. Beam energy and field size were 6 MV photon and 3 cm × 3 cm, respectively, in all three beam fields. For each field, 167 cGy was delivered and total 500 cGy was irradiated to TTA. All magnetic fields were applied in perpendicular direction to the beam paths. As SBM experiment, the magnetic field was generated by 5 cm × 5 cm sized neodymium magnets and magnetic strength at a mid-point of the MBM phantom was 0.3 T. After 3 fields irradiation for each phantom with or without magnetic field applied, absorbed doses were measured using the radiochromic films at the inner-surface and TTA. The radiochromic film was calibrated with research platform for a range of doses. All films were read out 24 hours after irradiation with a flatbed optical scanner.
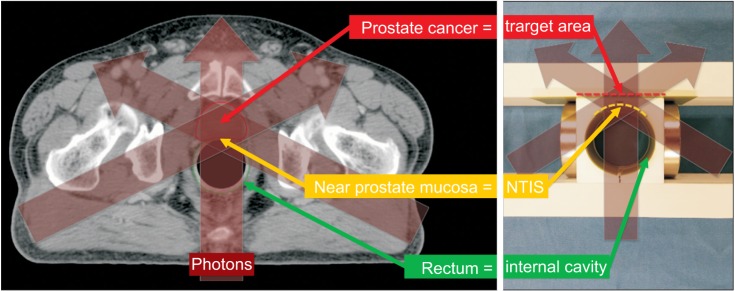
A computed tomography image of a case with prostate cancer shows spatial relation between prostate cancer and rectum (left). Components of multiple beam model phantom was matched with the case (right). Photon beam path is visualized with transparent red arrows on both images. NTIS, near target inner-surface.
Results
1. Single beam model experiment
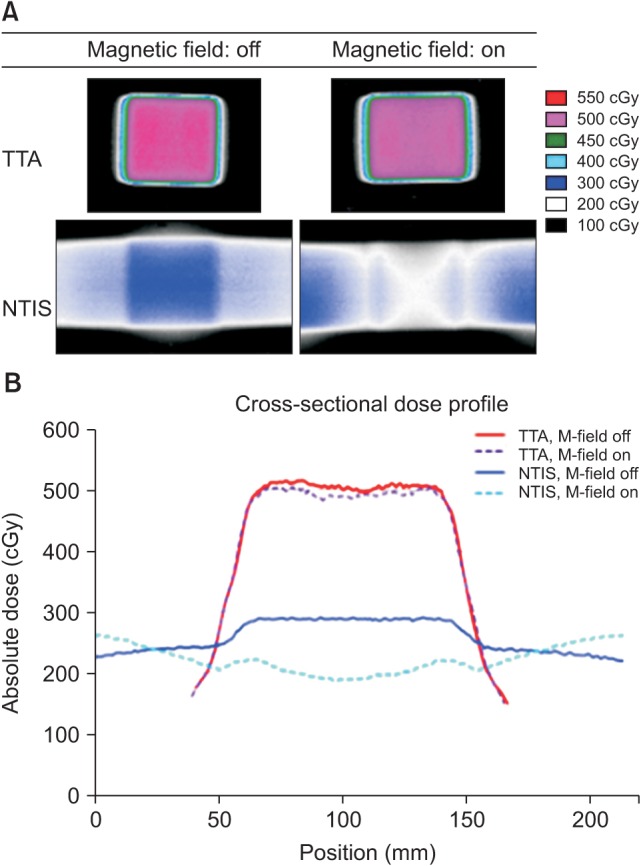
On longitudinal dose distribution images of SBM experiment, alteration of the dose distribution in the internal cavity was shown, with magnetic field applied (Fig. 4). With perpendicular magnetic field, dose distribution bent downward to radiation beam direction, comparing to data without magnetic field. In contrast to the internal cavity, pre-cavity area and TTA showed little changes of dose distributions with or without magnetic field. Depth dose distribution curve showed central axis dose difference with magnetic field application. Decrease of absorbed dose while radiation beam pass through air-filled internal cavity was more significant with magnetic field applied. At distal end of internal cavity (near TTA), absorbed dose of the experiments were 230 cGy and 320 cGy, with or without magnetic field, respectively. Therefore, dose decrease effect of magnetic field was 28.1%.

(A) Longitudinal central axis dose distribution of single beam model showed downward shifting of the radiation dose in the internal cavity, with magnetic field. (B) Radiation dose of near target internal cavity and surface portion of target tumor area (TTA) was decreased, while radiation dose in deep portion of TTA was little changed with magnetic field (red line, dose with magnetic field; blue line, dose without magnetic field).
2. Multiple beam model experiment
Cross sectional dose of NTIS was 190 cGy and 290 cGy, with or without magnetic field, respectively (Fig. 5). Dose decrease effect of magnetic field in NTIS was 34.5%. RT dose was measured at TTA, which 5 mm apart from NTIS, was 490 cGy and 500 cGy, with or without magnetic field, respectively. Dose difference of TTA owing to the magnetic field was 2.0%. Therefore, when TTA dose is standardized, RT dose reducing effect of magnetic field in NTIS was 33.1%. Meanwhile, dose increase effect with magnetic field was observed in other portion of the inner-surface (outside of NTIS).
Discussion and Conclusion
With physical advance in RT techniques, high precision RT became available. However, even with advanced RT techniques, when a target tumor is located near a critical organ which has low radiation tolerance, treating the target tumor with RT is challenging. Mucosal lined organ is known as one of radiosensitive organ, and tolerable RT dose is no more than 40 to 50 Gy in conventional fractionation [123]. Given that RT dose for tumor control is generally about 60 to 70 Gy, achieving tumor control without toxicities of mucosal lined organ (such as mucositis, ulceration) is still one of unsolved problems in radiation oncology.
With changes of radiation energy from kilovoltage to megavoltage, incidence and severity of skin complication is much decreased with RT, owing to a phenomenon known as 'skin-sparing effect'. It is well known that decrease of secondary electron deposition in the skin surface makes the skin-sparing effect of megavoltage RT. We hypothesized that if secondary electrons are removed in an internal cavity of a mucosal lined organ, the mucosa could be spared from high dose RT, similarly to the skin-sparing effect.
Lorentz force, generated by magnetic field, is known as physical interaction that only affects electrons, not photons. We thought that magnetic field could be utilized to remove secondary electrons in an air-filled internal cavity. Through this experiment, we confirmed that magnetic field could modify RT dose of NTIS without significant effect on post-surface TTA.
Diameters of human mucosal lined organs (such as oral cavity, esophagus, trachea, stomach, small bowel, and large bowel) are various; range about 2 to 7 cm. In our experiment, the diameter of the internal cavity was arbitrary selected as 4 cm to present feasibility of dose modulation with magnetic field. Because strength of magnetic field determine efficacy of secondary electron removal, different diameters of mucosal lined organs may need different strength of magnetic field. An organ with smaller internal diameter may need higher strength of magnetic field than that used in our experiment.
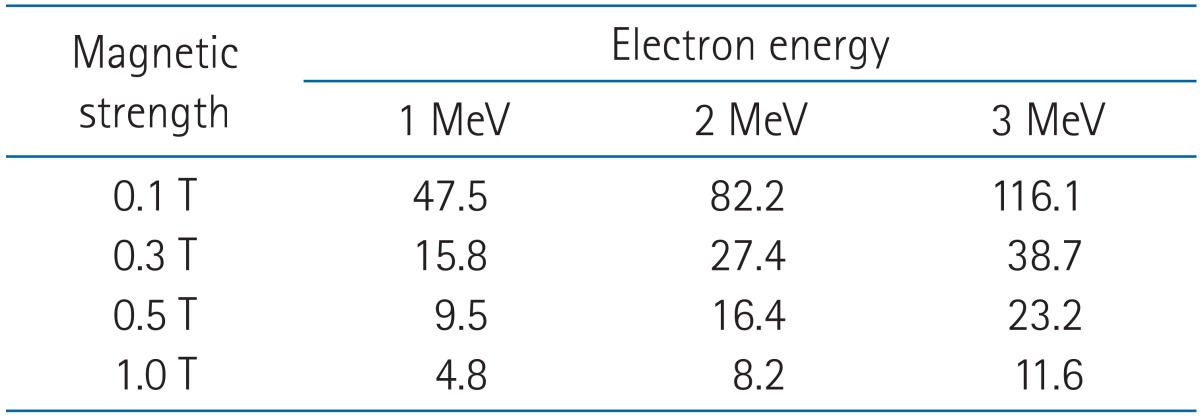
As shown in Fig. 1, the trajectory of secondary electron passing through internal cavity, is bent by Lorentz force of magnetic field. This arc-shaped electron trajectory's radius depends on the energy of the electrons and the strength of the magnetic field (Table 1). Insufficient strength of the magnetic field makes the radius of electron trajectory relatively big for the internal cavity. Consequently, the dose reduction effect with the magnetic field might be decreased. We presumed that if the radius of the electron trajectory and the internal cavity is same, the dose reduction effect in NTIS would be sufficient. Mean energy of photon is known as 1/3 of nominal photon energy [6]. Energy of secondary electrons has been evaluated using Monte Carlo simulation by other reports that distribution of the energy is mostly below 1/2 of nominal photon energy. And the mean energy of the secondary electrons is about 10% to 15% of the nominal photon energy, within the range of 6 to 15 MV [78]. Therefore, using 6 MV photon beam, we targeted to bend electrons whose energy is below 3 MeV in the current study. Given that the diameter of the internal cavity was 4 cm, magnetic strength of 0.3 T is sufficient for bending 3 MeV electron's trajectory (Table 1). Hence, photon beam energy of 6 MV and magnetic field strength of 0.3 T were chosen for the experiments of this study.
SBM experiment showed longitudinal dose distribution with or without magnetic field. Magnetic field which perpendicular to radiation beam, made motion of secondary electrons to bend laterally by Lorentz force. It was presented on longitudinal radiochromic film as downward shifting of the dose distribution. This bending effect of the secondary electrons prevents its deposition to forward direction inner-surface, which is NTIS. Therefore, RT dose of NTIS is decreased, meanwhile dose of other portion of inner-surface is increased.
Using longitudinal radiochromic film to measure absorbed dose of the internal cavity in SBM experiment could make the measurement over-estimated. Because of the film itself, the internal air cavity was not a true air cavity. So, this longitudinal measurement could only show tendency of the dose modulation. Actual RT dose and differences with using magnetic field could be obtained with cross-sectional film study, which performed in MBM experiment.
Dose of each points of the inner-surface is eventually 'zero-sum.' It is because secondary electrons of internal cavity are not eliminated, but repositioned. Electrons which could have been deposited on NTIS, are repositioned to other portion of the inner-surface. Therefore, dose of specific point could be decreased or increased, according to directions of both the photon beam and the magnetic field. Careful combination of photon beam and magnetic field is needed to draw intended dose modulation, especially when multiple beams are given. RT toxicity of mucosal lined organ has certain threshold dose, and damages made by RT of below toxicity threshold dose are generally restored completely. Therefore, even though low dose portion is increased, decreasing RT dose of near target high dose area might be important to reduce RT toxicity.
Prostate cancer is relatively common malignancy in which toxicity of rectal mucosa is one of mainly concerned adverse effects of RT [910]. To make more clinically relevant phantom model, MBM experiment simulated a case of prostate cancer, in which rectum (mucosal lined organ) is closed to prostate. Three different RT fields were used, and 100% of photon beam is irradiated to both NTIS and TTA. Dose reduction of NTIS was confirmed, as SBM experiment. RT dose of NTIS was decreased by 33.1% with magnetic field applied, when RT dose of TTA was standardized. If TTA is prescribed to receive 100% dose, only 38.8% of the prescription dose will be absorbed in NTIS with magnetic field. This magnetic RT dose modulation process might be applicable to patients with prostate cancer to reduce rectal toxicity.
The results of MBM experiments might be over-estimated and may not directly applicable to complex clinical situation in which more diverse directions of RT beam or intensity modulated RT is needed. But rather than experiments with clinically more relevant condition, we conducted simplified experiments to suggest this conceptual model of magnetic dose modulation, and to present its' beneficial effect as much as possible. Further study is needed to verify these initial results.
There has been reports showed effect of magnetic field on RT dose distribution [711121314]. Patterns of the effect on RT dose distribution were various with different strength of applied magnetic field. Relatively low strength (<1 T) of magnetic field only changed dose distribution of an air cavity and surface of a tissue density material [1112]. Dose distribution of internal portion of a tissue density material was significantly changed, when very high strength of magnetic field (>5 T) is applied [71314]. Magnetic field of our study was designed to modulate secondary electrons not in dense body tissue, but in the air-filled internal cavity. So, for this purpose we used relatively low strength of magnetic field in which maximum strength was 0.3 T. More effective RT dose modulation could be obtained by using stronger magnetic field than 0.3 T. But potent magnetic field could also induce significant unwanted dose increase in other portion of inner-surface (outside of NTIS), which is known as electron return effect [713]. Further research is required to find optimal magnetic field strength to RT dose modulation.
In this study, authors performed relatively small sized phantom experiments. Although the experiments showed promising results, there are limitations to applying magnetic dose modulation in actual clinical situation. Proper delivery of magnetic field to patient as well as shielding of magnetic field to prevent linear accelerator RT machine influenced by the magnetic field is important. Basically, similarly to diagnostic magnetic resonance imaging (MRI) machine, the magnetic field could be generated in external space around patient treatment area. But unlikely to diagnostic MRI which requires large area of homogenous magnetic field, magnetic RT dose modulation of this study may need smaller local magnetic field in the treatment area. Smaller local magnetic field might be generated with smaller magnetic device, and effect of magnetic field in surrounding area is probably also smaller. This aspect could make shielding linear accelerator RT machine from the magnetic field more possible.
In clinical situations, RT is delivered with various factors, such as beam direction, beam energy, field size, RT dose, and application of intensity modulation. According to various directions of RT beam field, directions of magnetic field for dose modulation should also be various. Spatial limitation around a RT machine and a patient may limit installation of the magnetic device. And the other factors may also affect magnetic field design. Optimization of magnetic field design is required for clinical application of this concept of magnetic dose modulation.
This approach of magnetic RT dose modulation needs more intention when treating tumors located at internal surface (i.e., mucosa), such as esophageal cancer, rectal cancer, and glottic cancer. Because RT dose reduction in the internal surface could lead to tumor dose reduction, and compromise tumor control probability. The tumor control probability would be better when RT is delivered without magnetic field.
It is well known that magnetic field could affect RT, though Lorentz force. By far we know, several previous studies have reported that high strength magnetic field could deteriorate RT dose distribution [7141516]. However, our study showed that relatively low strength magnetic field with a specific condition could modulate RT dose in a beneficial direction.
In conclusion, this phantom experiment showed that near target mucosal dose could be reduced by low strength local magnetic field, without significant effect on target tumor dose.
Acknowledgments
This work was supported by the National Research Foundation of Korea (NRF) funded by the Korean government (No. 2014R1A1A2058154).
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.