 |
 |
AbstractPurposeThe purpose of this study is to compare the dosimetry of electron beam (EB) plans and three-dimensional helical tomotherapy (3DHT) plans for the patients with left-sided breast cancer, who underwent breast conserving surgery.
Materials and MethodsWe selected total of 15 patients based on the location of tumor, as following subsite: subareolar, upper outer, upper inner, lower lateral, and lower medial quadrants. The clinical target volume (CTV) was defined as the area of architectural distortion surrounded by surgical clip plus 1 cm margin. The conformity index (CI), homogeneity index (HI), quality of coverage (QC) and dose-volume parameters for the CTV, and organ at risk (OAR) were calculated. The following treatment techniques were assessed: single conformal EB plans; 3DHT plans with directional block of left anterior descending artery (LAD); and 3DHT plans with complete block of LAD.
Results3DHT plans, regardless of type of LAD block, showed significantly better CI, HI, and QC for the CTVs, compared with the EB plans. However, 3DHT plans showed increase in the V1Gy at skin, left lung, and left breast. In terms of LAD, 3DHT plans with complete block of LAD showed extremely low dose, while dose increase in other OARs were observed, when compared with other plans. EB plans showed the worst conformity at upper outer quadrants of tumor bed site.
IntroductionThe current standard treatment for early breast cancer is breast-conserving surgery, followed by whole-breast irradiation and tumor-bed boost irradiation [1]. The benefit of the additional tumor bed boost, which has been shown to decrease local recurrence rates, has been supported by numbers of randomized studies [234]. The single-field electron beam (EB) plan has been commonly used to deliver a tumor bed boost with a characteristic sharp dose drop-off beyond the target volume. Because of the unsatisfactory target coverage of EB plan in some cases, tumor bed boosting with a photon beam was studied and has shown superior target coverage than EB plan [56]. On the other hand, photon boost have been discouraged because of excess doses to normal tissues such as lungs and heart [7]. Particularly, it is important of efforts to reduce dose to left anterior descending coronary artery (LAD) because clinical data showed that radiation exposure of the heart during radiotherapy (RT) for breast cancer increases the rate of ischemic heart disease [8].
Modern TomoTherapy machine (Accuray Inc., Sunnyvale, CA, USA) provides various types of radiation delivery [9]. Users can select three-dimensional conformal radiotherapy (3D-CRT) by direct or helical beam as well as intensity-modulated radiotherapy (IMRT) depending on size, site, and type of tumor. We speculate that three-dimensional helical tomotherapy (3DHT) might be a favorable method for boost RT to overcome poor target coverage of EB plans and immoderate irradiation of normal tissues in photon plans. Therefore, we investigated the usefulness of 3DHT plans for boost RT by examining the dosimetric benefit of target coverage and reducing LAD dose.
Materials and Methods1. Patient selectionTo find the dosimetric differences according to tumor site including subareolar, upper inner, upper outer, lower medial, and lower lateral quadrants, we selected 3 patients for each group. Total of 15 patients who received adjuvant RT were identified from June 2010 to June 2011. Included criteria were as follows: 1) patients with stage I/IIA left-sided breast cancer; 2) patient who had received definitive RT following the breast conserving surgery; and 3) patient who had surgical clips at tumor bed.
2. Target volume delineationAnatomic information from the computed tomography (CT) scan was used to define the volumes at risk and normal structures. The tumor bed was defined as the area of architectural distortion combined with the location of surgical clips. The clinical target volume (CTV) was delineated with a 1 cm margin from the tumor bed, excluding the pectoralis muscles, chest wall, and a 5-mm depth beneath the skin. EB plans were designed by block margin with 1 cm margin from CTV because of beam penumbra and block edge effects.
Organ at risk (OAR) included left breast, left lung, right breast, right lung, skin, and LAD. We delineated breast boundary according to the caudal edge of the sternoclavicular junction as cranial border, the intermammary sulcus as caudal border, the major pectoralis muscle as dorsal border, the axillary vessels as lateral border and the ipsilateral edge of sternum as medial border [10]. The skin was defined to be 5 mm thick from surface of body. The contouring of the LAD was attempted on each CT image using the heart atlas proposed by Feng et al. [11].
3. Treatment planningEB and 3DHT plans for boost RT were compared in each case. The EB plans used a single electron field with a central axis perpendicular to the CTV. In order for the CTV to be covered by the 90% isodose line, we selected one of electron energy among 6, 9, and 12 MeV depending on the depth of the CTV. We did not apply the bolus for EB plans because most patients had deep-seated CTV. The overall goal was to deliver 10 Gy to the CTV at 2 Gy per fraction. We performed the EB plans using a radiation planning program (Pinnacle3 v7.8c; Philips Heathcare, Andover, MA, USA). 3DHT plans were generated using the TomoTherapy planning system (Accuray Inc.). We used helical tomotherapy which is a radiation delivery modality that delivers a modulated fan beam using a 6-MV linear accelerator mounted on a ring gantry that rotates around patient through the gantry bore. A jaw of 2.5 cm width was used for all plans. 3DHT beam angles were automatically selected for delivery of the prescribed dose in target. And 3DHT plans have two constraint options against contour: directional block and complete block. Directional block avoids the direct beamlet, while permitting exit beamlet. On the other hand, complete block does not allow entry nor exit of beamlet. These plans are different from IMRT. IMRT plans in TomoTherapy planning system should have various importance and weighted penalties according to constraints of OARs, whereas 3DHT plans can select type of block option only, as we mentioned above. TomoTherapy provided two 3D-CRT mode as well as IMRT. Users can select direct beam or helical beam into 3D-CRT mode depending on target. Among them, we used helical beam in 3D-CRT mode of TomoTherapy.
We created three artificial structures applied to directional block to protect OARs: block 1 for contralateral breast; block 2 for ipsilateral lung; and block 3 for minimizing irradiated dose on other OARs (i.e., ipsilateral breast, skin). Block 1 was created at mid-sternum below skin surface in coverage of CTV at 5 mm thickness. The block 2 and 3 were made each slice by parallel planes of 4 cm distance from CTV. These blocks were schematic contouring for easier judgment of block effect. And we planned constraint of LAD for minimizing LAD dose in 3DHT plans. We compared 3DHT plans using directional block with complete block of LAD (Fig. 1). A prescription dose of 10 Gy in 5 fractions was used for each plan with the optimization goal of delivering the prescription dose to 90% of the CTV.
4. Dosimetric analysisThe EB and two 3DHT plans for three patients according to each tumor site were compared via dose-volume histograms (DVH). Target coverage was assessed by comparing the homogeneity index (HI) and conformity index (CI) of the plan. The HI was defined as the ratio of the dose received by 5% volume of the CTV to the dose received by 95% of CTV (i.e., HI = D5% / D95%). The CI was defined as the ratio between the volume receiving at least 95% of the prescribed dose and the volume of the CTV (i.e., CI = V95% / CTV). For comparing of target coverage quality, quality control (QC) was defined by the ratio between the irradiated minimum dose and the prescribed dose for the CTV (i.e., QC = Dmin / D).
OAR sparing was evaluated by comparing the mean dose as well as the dose-volume parameters. A set of appropriate V-values such as V1Gy, V3Gy, and V8Gy (relative volumes receiving ≥1, ≥3, or ≥8 Gy of the prescribed dose, respectively) were also calculated. All plans were normalized to deliver 10 Gy within the 95% isodose line after completing RT for the purpose of dosimetric analysis.
5. Statistical analysisOne-way analysis of variance test was used to compare dosimetric differences among plans. All statistical tests were two-sided, and were performed using SPSS software program ver. 20.0 (IBM, Armonk, NY, USA). When comparing the data series, the mean values were confronted in all cases, a significance level of p < 0.05 was considered to be a significant difference.
Results1. Target coverageThe mean CTV volume for all patients was 59.27 cm3 (range, 23.71 to 89.30 cm3). In 3DHT plans, treatment time was 168 ± 54 seconds and monitor unit (MU) was 2,468 ± 763 MU. Meanwhile, EB plans showed 26 ± 12 seconds in treatment time and 227 ± 38 MU in MU. As shown in Table 1, the CTV coverage of both 3DHT plans with directional block or complete block of LAD was superior to that of EB plans. The 3DHT plans provided superior CI, HI, QC, Dmean, and V95% for the CTVs, compared to the EB plans. EB plans had less target coverage compared to 3DHT plans but had no overdose to prescribed dose. On the other hand, 3DHT plans led to consistently higher (V107%), especially with the complete block of LAD.
The dosimetric parameters according to tumor site were evaluated (Fig. 2). Dose distributions were perturbed by skin surface in EB plans, especially, at upper outer quadrant. CI of EB plans at upper outer quadrant showed the lowest among other quadrants. Moreover, EB plans have poor HI at all sites. Particularly, HI on upper inner and lower lateral quadrant are enhanced. In contrast, HT plans with directional and complete block of LAD were presented with better CI and HI regardless of sites. In cases of lower medial quadrant, 3DHT plans with directional block of LAD showed good coverage from QC.
2. Sparing OARs
Table 2 provides the numerical findings from the DVH analysis of the OARs. EB plans showed lower Dmean, D1% and V1Gy of skin compared to the 3DHT plans. Left lung and left breast also had the lowest Dmean in the EB plans. Although quality of the EB plans fluctuated among the patients and was affected by the target depth, EB plans showed superior OAR sparing, except LAD, than 3DHT plans with both directional block and complete block of LAD. On the other hand, 3DHT plans with complete block of LAD have understandably successful LAD sparing. 3DHT plans with directional block of LAD showed overdose at LAD compared with EB in all cases. Low-dose volume of LAD was also increased in 3DHT with directional block in all cases (Table 3).
EB plans had no irradiated field at right lung and right breast. However, 3DHT plans, regardless of block type, showed low dose exposure in spite of less than 1 Gy of mean dose (Table 2). 3DHT plans with directional block of LAD showed mean dose of 0.25 ± 0.12 Gy of right lung and 0.30 ± 0.13 Gy of right breast. 3DHT plans with complete block of LAD showed mean dose of 0.21 ± 0.10 Gy of right lung and 0.27 ± 0.16 Gy of right breast. However, we found that there were no statistically significant differences among Dmean, D1%, and V3Gy to be compared with directional and complete block of LAD.
In terms of skin dose, the 3DHT plans increased the Dmean and V1Gy in comparison to the EB plans. A similar trend was observed on the left lung and left breast. Although Dmean of lung was lower in EB plans, V3Gy representing the high-dose volume was higher than the 3DHT plans (Table 2). In contrast, the Dmean, D1%, and D50% of the left breast were higher in the 3DHT plans than in the EB plans. In all plans, we found there was no more than 110% of the prescription dose.
We found that irradiated LAD volume was increased at subareolar, upper inner and lower medial quadrant due to anatomical direction of LAD. Particularly, in cases with tumor bed at lower medial quadrant, V1Gy of LAD was 100% (Fig. 2). LAD doses in all cases were extremely low in 3DHT plans with complete block of LAD. However, these plans showed increased irradiated dose of left breast (Fig. 3).
Discussion and ConclusionWe sought to evaluate dosimetric analysis of three different techniques for boost plans. We found that the 3DHT plans, regardless of block type of LAD, improved dose homogeneity compared with EB plans. 3DHT plans showed increased low-dose volume of OARs in comparison with EB plans. In terms of LAD, 3DHT plans with complete block of LAD had significant LAD sparing from boost radiation, while they showed dose increase in left breast.
Although availability of 3DHT is proven by several studies [1213], there is little evidence of usefulness of 3DHT for breast boost RT in our knowledge. In 3DHT, the gantry is continuously rotated around the patient with the multileaf collimator position calculated approximately every 7° or 51 times/rotation as the patient slowly moves longitudinally past the fan beam. 3DHT can achieve highly conformal dose distribution at the cost of delivering a low dose of radiation to a large volume of coplanar normal tissues. Gantry angles can be directionally or completely blocked in the treatment-planning optimization to minimize entry and/or exit dose to OAR [14]. We adapted these blocks to minimize LAD dose.
In our study, 3DHT plans showed better target coverage compared with EB plans. In previous studies, photon beam plans showed superior target coverage than EB plans and 3DHT plans were demonstrated better target coverage than photon beam plans. Park and Kim [15] reported that photon plans were superior to EB plans in terms of target coverage, even high-dose volume sparing in OAR for boost irradiation. And Goddu et al. [16] reported that tomotherapy IMRT plans provided better dose conformity and homogeneity than the three-dimensional plans for left-sided breast cancer. However, studies about dosimetric analysis of tomotherapy IMRT plans for breast cancer showed 107% to 114% of average hotspots [1617]. Our study found that the average hotspots were 108% to 113% in 3DHT, while the other parameters of target coverage were favorable. Therefore, in terms of target coverage, 3DHT might be an alternative tool of tomotherapy IMRT.
To find out difference in target coverage according to subsite, we separately analyzed the irradiated dose to tumor bed site. EB plans of all subsites showed poorer target coverage compared with 3DHT plans. Especially, EB plans of tumor beds at upper outer quadrant showed the lowest values of conformity because of thickness change inside the target volume and irregular surface of skin by axillary fold. The target coverage of EB plans might be influenced by thickness to target and the irradiated surface.
Oxford meta-analyses found increased risks of coronary heart disease for irradiated patients compared with non-irradiated ones, or for patients treated to left breast compared to those treated to the right side [81819]. Another report demonstrated that the rate of cardiovascular mortality increased in patients who received RT of inner-quadrants [20].
In our study, mean dose of LAD was higher at subareolar, upper inner, and lower medial quadrants compared with upper outer and lower lateral quadrants of tumor site in EB plans. EB plans of tumor beds at upper outer quadrant showed the lowest dose at LAD, probably because of the LAD anatomy. On the other hand, 3DHT plans with directional block of LAD showed higher mean dose of LAD in all subsites compared with EB plans. Moreover, 3DHT plans with directional block showed higher V1Gy and V3Gy of LAD at all quadrants of tumor site except subareolar. Although 3DHT plans with complete block of LAD showed the lowest dose of LAD in all subsites, these plans increased mean dose of left breast. Besides, right breast and right lung also had low dose radiation on 3DHT plans.
The other report showed low dose exposure of breast increasing secondary breast cancer [21]. They demonstrated that women younger than 40 years who received more than 1 Gy of radiation dose to the contralateral breast had an elevated, long-term risk of developing a second primary contralateral breast cancer. In our study, mean dose of right breast was less than 1 Gy; 0.3 ± 0.13 Gy in 3DHT plans with directional block and 0.27 ± 0.16 in 3DHT plans with complete block. Although the clinical impact of additional low dose at contralateral breast is unclear for breast boost RT, the dose exposure for the right breast and lung was acceptable in 3DHT plans according dose limitations for normal tissues of RTOG [22].
3DHT plans, regardless of block type of LAD, had lower D50% of skin than EB plans (Table 2). In comparison with EB plans and photon beam plans in boost irradiation of breast cancer, the high-dose volume to the skin increased EB plans because of skin-sparing effect of photon [15]. However, we found that irradiated skin dose in 3DHT plans was increased compared with EB plans. In previous study, chest wall treatment plans from tomotherapy using by IMRT option showed higher skin dose than tangential delivery technique [23]. They explained the reasons for the higher skin dose are as follows: 1) the shallower dmax by slightly lower mean energy; 2) the shallow delivery angles; and 3) the smaller source-axis distance of the tomotherapy machine. These might be the causes of our findings.
In conclusion, 3DHT plans permitted more optimal target coverage than EB plans for boost RT in breast cancer patients. EB plans might be more preferred for OAR sparing except for LAD. 3DHT plans are preferable in upper outer quadrant of tumor beds for better target coverage. 3DHT plans with complete block of LAD might be considered in cases of subareolar, upper inner, lower lateral quadrants of tumor site to reduce the dose of LAD for breast cancer patients with cardiac morbidity.
References1. Halperin EC, Perez CA, Brady LW. Perez and Brady's principles and practice of radiation oncology. 5th ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2008.
2. Collette S, Collette L, Budiharto T, et al. Predictors of the risk of fibrosis at 10 years after breast conserving therapy for early breast cancer: a study based on the EORTC Trial 22881-10882 'boost versus no boost'. Eur J Cancer 2008;44:2587–2599, PMID: 18757193.
3. Romestaing P, Lehingue Y, Carrie C, et al. Role of a 10-Gy boost in the conservative treatment of early breast cancer: results of a randomized clinical trial in Lyon, France. J Clin Oncol 1997;15:963–968, PMID: 9060534.
4. Kirova YM, Fournier-Bidoz N, Servois V, et al. How to boost the breast tumor bed? A multidisciplinary approach in eight steps. Int J Radiat Oncol Biol Phys 2008;72:494–500, PMID: 18374516.
5. Kovacs A, Hadjiev J, Lakosi F, et al. Comparison of photon with electron boost in treatment of early stage breast cancer. Pathol Oncol Res 2008;14:193–197, PMID: 18347930.
6. Toscas JI, Linero D, Rubio I, et al. Boosting the tumor bed from deep-seated tumors in early-stage breast cancer: a planning study between electron, photon, and proton beams. Radiother Oncol 2010;96:192–198, PMID: 20538361.
7. Quill T, Abair T, Garcia K. The American Society of Clinical Oncology 2009 Breast Cancer Symposium, San Francisco, CA, October 8-10, 2009. Clin Breast Cancer 2009;9:213–218, PMID: 19933075.
8. Darby SC, Ewertz M, McGale P, et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med 2013;368:987–998, PMID: 23484825.
9. Gotoh S. Revolution in radiation therapy: TomoTherapy HI-ART system. Nihon Hoshasen Gijutsu Gakkai Zasshi 2006;62:1611–1619, PMID: 17233123.
10. Nielsen MH, Berg M, Pedersen AN, et al. Delineation of target volumes and organs at risk in adjuvant radiotherapy of early breast cancer: national guidelines and contouring atlas by the Danish Breast Cancer Cooperative Group. Acta Oncol 2013;52:703–710, PMID: 23421926.
11. Feng M, Moran JM, Koelling T, et al. Development and validation of a heart atlas to study cardiac exposure to radiation following treatment for breast cancer. Int J Radiat Oncol Biol Phys 2011;79:10–18, PMID: 20421148.
12. Reynders T, Tournel K, De Coninck P, et al. Dosimetric assessment of static and helical TomoTherapy in the clinical implementation of breast cancer treatments. Radiother Oncol 2009;93:71–79, PMID: 19682758.
13. Kainz K, White J, Herman J, Li XA. Investigation of helical tomotherapy for partial-breast irradiation of prone-positioned patients. Int J Radiat Oncol Biol Phys 2009;74:275–282, PMID: 19362247.
14. Jeraj R, Mackie TR, Balog J, et al. Radiation characteristics of helical tomotherapy. Med Phys 2004;31:396–404, PMID: 15000626.
15. Park SH, Kim JC. Comparison of electron and X-ray beams for tumor bed boost irradiation in breast-conserving treatment. J Breast Cancer 2013;16:300–307, PMID: 24155759.
16. Goddu SM, Chaudhari S, Mamalui-Hunter M, et al. Helical tomotherapy planning for left-sided breast cancer patients with positive lymph nodes: comparison to conventional multiport breast technique. Int J Radiat Oncol Biol Phys 2009;73:1243–1251, PMID: 19251096.
17. Fogliata A, Nicolini G, Alber M, et al. IMRT for breast. a planning study. Radiother Oncol 2005;76:300–310, PMID: 16153730.
18. Early Breast Cancer Trialists' Collaborative Group. Favourable and unfavourable effects on long-term survival of radiotherapy for early breast cancer: an overview of the randomised trials. Lancet 2000;355:1757–1770, PMID: 10832826.
19. Clarke M, Collins R, Darby S, et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet 2005;366:2087–2106, PMID: 16360786.
20. Bouchardy C, Rapiti E, Usel M, et al. Excess of cardiovascular mortality among node-negative breast cancer patients irradiated for inner-quadrant tumors. Ann Oncol 2010;21:459–465, PMID: 19703922.
21. Stovall M, Smith SA, Langholz BM, et al. Dose to the contralateral breast from radiotherapy and risk of second primary breast cancer in the WECARE study. Int J Radiat Oncol Biol Phys 2008;72:1021–1030, PMID: 18556141.
22. Hiatt JR, Evans SB, Price LL, Cardarelli GA, Dipetrillo TA, Wazer DE. Dose-modeling study to compare external beam techniques from protocol NSABP B-39/RTOG 0413 for patients with highly unfavorable cardiac anatomy. Int J Radiat Oncol Biol Phys 2006;65:1368–1374, PMID: 16863924.
23. Javedan K, Zhang G, Mueller R, Harris E, Berk L, Forster K. Skin dose study of chest wall treatment with tomotherapy. Jpn J Radiol 2009;27:355–362, PMID: 19943146.
Fig. 1Isodose distribution in axial planes. (A) Electron beam plan. (B) Helical tomotherapy plan with directional block of left anterior descending coronary artery. (C) Helical tomotherapy plan with complete block of left anterior descending coronary artery. The black arrow indicates the left anterior descending coronary artery.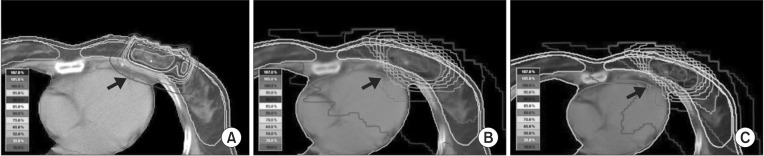
Fig. 2Target coverage according to quadrant of tumor site. CI, conformity index; HI, homogeneity index; QC, quality of coverage; HT (D), helical tomotherapy with directional block of left anterior descending coronary artery; HT (C), helical tomotherapy with complete block of left anterior descending coronary artery.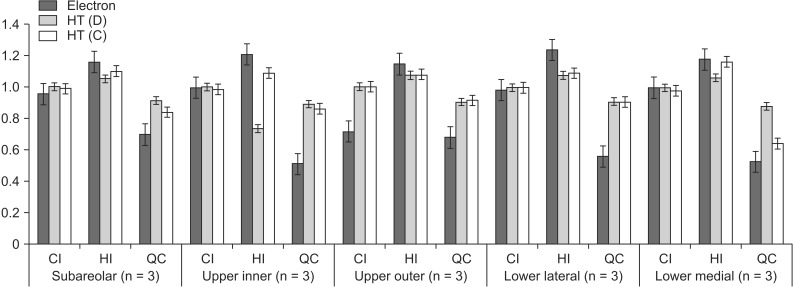
Fig. 3Mean dose of LAD and left breast according to quadrant of tumor site. LAD, left anterior descending coronary artery; HT (D), helical tomotherapy with directional block of LAD; HT (C), helical tomotherapy with complete block of LAD.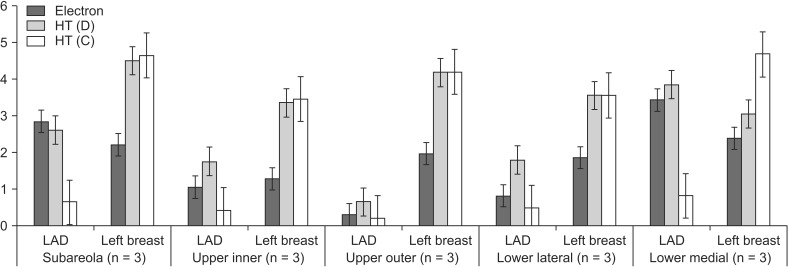
Table 1Target coverage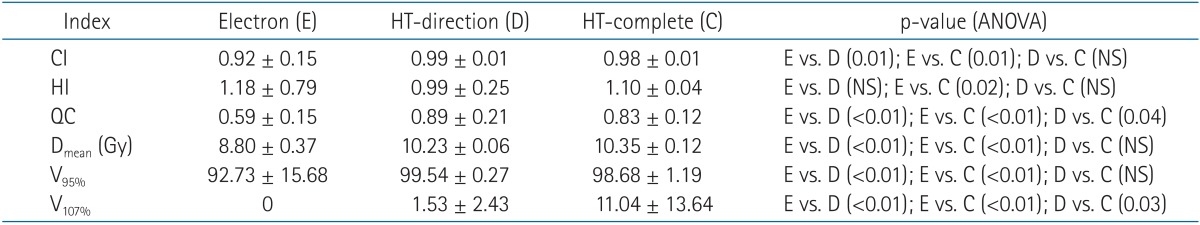 Values are presented as mean ± standard deviation. HT-direction, helical tomotherapy with directional block of LAD; HT-complete, helical tomotherapy with complete block of LAD; CI, conformity index; NS, not statistically significant; HI, homogeneity index; QC, quality of coverage; Dmean, mean dose; V95%, volume receiving ≥95% of prescribed dose; V107%, volume receiving ≥107% of prescribed dose; LAD, left anterior descending coronary artery. Table 2Doses to organs at risk (n = 15)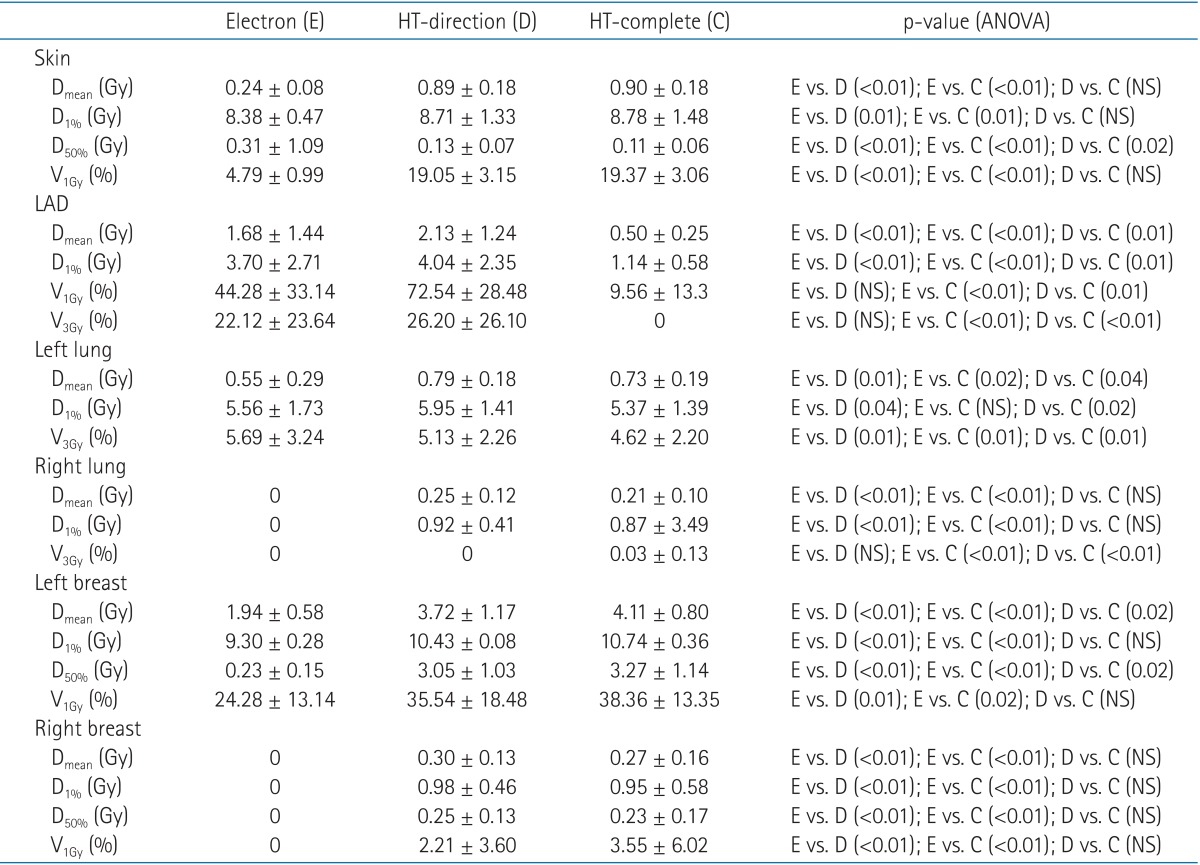 Values are presented as mean ± standard deviation. HT-direction, helical tomotherapy with directional block of LAD; HT-complete, helical tomotherapy with complete block of LAD; Dmean, mean dose; D1%, dose receiving ≥1% volume of CTV; D50%, dose receiving ≥50% volume of CTV; V1Gy, volume receiving ≥1 Gy of prescribed dose; V3Gy, volume receiving ≥3 Gy of prescribed dose; NS, not statistically significant; LAD, left anterior descending coronary artery; CTV, clinical target volume. Table 3Doses of left anterior descending artery according to quadrant of tumor site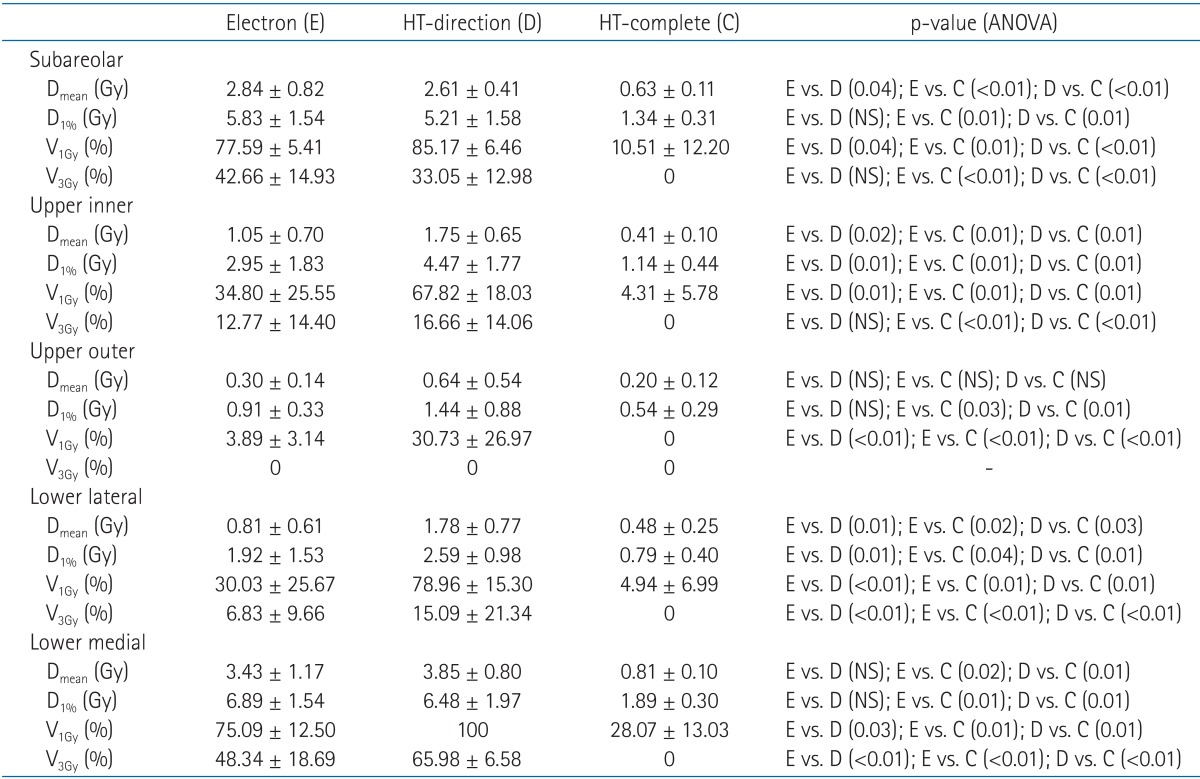 Values are presented as mean ± standard deviation. HT-direction, helical tomotherapy with directional block of LAD; HT-complete, helical tomotherapy with complete block of LAD; Dmean, mean dose; D1%, dose receiving ≥1% volume of CTV; V1Gy, volume receiving ≥1 Gy of prescribed dose; V3Gy, volume receiving ≥3 Gy of prescribed dose; NS, not statistically significant; LAD, left anterior descending coronary artery; CTV, clinical target volume. |
|
||||||||||||||||||||||||||||||||||||||||||||

 |
 |