Adverse effect of excess body weight on survival in cervical cancer patients after surgery and radiotherapy
Article information
Abstract
Purpose
This study aimed to assess the effects of body mass index (BMI) on survival in cervical cancer patients who had undergone surgery and radiotherapy (RT).
Materials and Methods
We retrospectively reviewed the medical records of 70 cervical cancer patients who underwent surgery and RT from 2007 to 2012. Among them, 40 patients (57.1%) had pelvic lymph node metastases at the time of diagnosis. Sixty-seven patients (95.7%) had received chemotherapy. All patients had undergone surgery and postoperative RT. Median BMI of patients was 22.8 kg/m2 (range, 17.7 to 35.9 kg/m2).
Results
The median duration of follow-up was 52.3 months (range, 16 to 107 months). Twenty-four patients (34.3%) showed recurrence. Local failure, regional lymph nodal failure, and distant failure occurred in 4 (5.7%), 6 (8.6%), and 17 (24.3%) patients, respectively. The 5-year actuarial pelvic control rate was 83.4%. The 5-year cancer-specific survival (CSS) and disease-free survival (DFS) rates were 85.1% and 65.0%, respectively. The presence of pelvic lymph node metastases (n = 30) and being overweight or obese (n = 34, BMI ≥ 23 kg/m2) were poor prognostic factors for CSS (p = 0.003 and p = 0.045, respectively). Of these, pelvic lymph node metastasis was an independent prognostic factor (p = 0.030) for CSS.
Conclusion
Overweight or obese cervical cancer patients showed poorer survival outcomes than normal weight or underweight patients. Weight control seems to be important in cervical cancer patients to improve clinical outcomes.
Introduction
Cervical cancer is one of the most common cancers in women worldwide, even though its mortality rate has declined due to vaccination and active screening programs [1,2]. Generally, stage I-IIa cervical cancer patients are managed through radical hysterectomy. Radiotherapy (RT) without surgery can be used to treat all stages of cervical cancer, with a modest overall survival rate of about 60% for stage II disease. Although curative RT is the treatment of choice for the International Federation of Gynecology and Obstetrics (FIGO) stage IIb cervical cancer [3], surgical resection is often performed before RT. Compared to RT, surgery is advantageous for younger women who wish to preserve ovarian function. Moreover, surgical resection provides accurate information about the stage of the cancer. After surgical resection, additional postoperative RT is generally recommended in patients with pelvic lymph node metastases, invasion of paracervical tissue, deep cervical invasion, or positive surgical margins, in order to improve survival outcomes.
More evidence about the relationship between cancer progression and overweight or obesity is available these days [4-6]. According to recent reports, cancer is primarily a metabolic disease [7]. Several clinical studies [5,6,8] have explained the association between obesity and incidence of cancers such as colon cancer, breast cancer, endometrial cancer, cervical cancer, and ovarian cancer. In addition, low levels of adiponectin (an adipocyte-specific protein, which involves insulin resistance) are related to the occurrence of cancers that typically affect women [4].
Occurrence of cervical cancer is related to patient body mass index (BMI) according to recent reports [9-13]. Though the main risk factor for occurrence of cervical cancer is infection by human papillomavirus (HPV) [14], other factors are also involved in the development of cervical cancer. Body weight and calorie intake are shown to influence cervical cancer development. Clark et al. [13] recently reported that extremes of body weight related to reduced survival in cervical cancer patients. Ahn et al. [9] reported that triglyceride levels and impaired fasting glucose levels are prognostic factors for recurrence-free survival in early-stage cervical cancer patients. If being overweight or obese influences cancer treatment outcomes, lifestyle modifications [15] can be important for patients who undergo cancer treatment, not only as primary prevention but also as secondary preventative measure after treatment.
In this study, we evaluated the effect of BMI on the prognosis of Asian cervical cancer patients, after they had undergone surgery and RT. The primary end point of this study was cancer-specific survival (CSS). We hypothesized that obese or overweight cervical cancer patients would have poor treatment outcomes compared to normal or underweight patients.
Materials and Methods
We retrospectively evaluated the medical records of 70 patients, who were clinically diagnosed with FIGO stage IIb cervical cancer and treated with surgery and RT from March 2007 to September 2012 at Inje University Busan Paik Hospital. This study was approved by the ethics committee of Inje University Busan Paik Hospital. The patients who had received definitive RT without radical surgery were excluded for evaluation. We did not evaluate patients who had abdominal para-aortic or inguinal lymph node metastases at the time of diagnosis, who underwent inappropriate resection (total hysterectomy or trachelectomy) for cancer treatment, who died, or who were lost to follow-up within 12 months of diagnosis.
Obesity and overweight were defined according to Asian BMI classification. BMI was obtained by dividing body weight (kg) by height (m) squared. Normal weight is defined as a BMI equal or greater than 18.5 kg/m2 and less than 23 kg/m2. BMI equal to or greater than 23 kg/m2 is considered overweight; above 25 kg/m2, obese; below 18.5 kg/m2, underweight. Information for the patients’ body weight and height was obtained from the electronic anesthesia records on the day of surgery.
All patients received surgical resection as follows; radical abdominal hysterectomy (n = 52), radical abdominal hysterectomy with bilateral salpingo-oophorectomy (n = 12), and radical abdominal hysterectomy with bilateral pelvic lymphadenectomy (n = 6).
Three-dimensional conformal RT was administered to all patients. The daily dose of external beam RT was 1.8 Gy, which was delivered via a four-field box technique to the pelvis for up to 50.4 Gy (range, 45 to 50.4 Gy). An additional external beam boost to tumor bed was administered to 3 patients with 3.6–9 Gy. High-dose-rate intracavitary radiation therapy (ICR) was performed in 23 patients (32.9%), with a pathologically high risk of treatment failure, such as a positive surgical resection margin. The dose of ICR to point A was 10–15 Gy for postoperative RT and was delivered as 3–5 Gy per fraction.
Characteristics of the patients are summarized in Table 1. The median age of the patients was 54.5 years (range, 35 to 77 years). Chemotherapy was administered in 67 patients (95.7%). The chemotherapy regimen consisted of cisplatin (n = 60), 5-fluorouracil (n = 66), or both.
Pelvic failure (in-field failure) was defined as recurrence or progression of cancer at the stump, or pelvic (regional) lymph node failure, or a combination of these characteristics. Pelvic control was calculated from the date of pathologic diagnosis to the date of intra-pelvic failure or of last follow-up. Disease-free survival (DFS) was calculated from the date of pathologic diagnosis to the date of overall progression (intra-pelvic or distant failure) or of final follow-up. CSS was measured from the date of diagnosis to the date of expiration due to cervical cancer progression or date of final follow-up.
Statistical analysis was performed using SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA). A p-value of less than 0.05 was considered statistically significant. The chi-square test was used to compare two groups to find the clinical factors related to BMI and to estimate the effects of excess body weight on treatment failure. The Kaplan-Meier method was used to estimate pelvic control, DFS, and CSS. Rates of survival and pelvic control were compared using a log-rank test. The Cox regression hazard model was used to assess independent prognostic factors for survival.
Results
1. Pattern of failure
The median duration of follow-up was 52.3 months (range, 16 to 107 months). Overall, 24 patients experienced recurrence. Ten patients (14.3%) showed intra-pelvic recurrence (in-field failure, including 4 local failures and 6 pelvic lymph nodal failures) and 17 patients (21.4%) experienced distant failure. Three patients showed both intra-pelvic recurrence and distant failure during the follow-up period. The most frequent distant failure sites were the lungs (n = 3). Nine patients (12.9%) died during the follow-up period, because of disease progression.
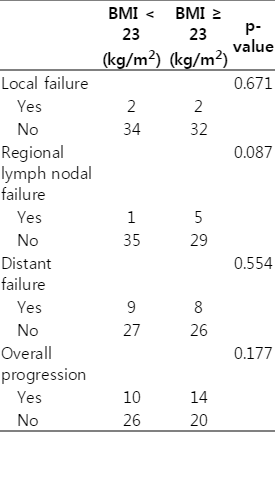
Table 2 shows pattern of failure correlated with BMI values (BMI < 23 kg/m2 or BMI ≥ 23 kg/m2). Local failure (operation site or marginal failure), pelvic failure (in-field failure, including local failure and regional lymph nodal failure), and overall progression were not significantly different between the overweight or obese patients (BMI ≥ 23 kg/m2, n = 34) and the normal weight or underweight patients (p = 0.224, p = 0.224, and p = 0.124, respectively). However, regional lymph nodal failure tended to be higher in the overweight or obese patients than in normal or underweight patients (p = 0.087).
2. Actuarial pelvic control
The 5-year actuarial pelvic control rate was 83.4%. Fig. 1 shows the pelvic control, DFS, and CSS. Underweight or normal weight patients did not have a better actuarial pelvic control rate than overweight or obese patients (p = 0.123, 5-year pelvic control, BMI < 23 kg/m2 [91.5%] vs. BMI ≥ 23 kg/m2 [73.2%]).
3. Survival analysis
The 5-year CSS and DFS rates were 85.1% and 65.0%, respectively (Fig. 1). In further analysis, the 5-year DFS rate was not differentiated by obesity or overweight (p = 0.224).
Table 3 shows the prognostic factors for CSS. Overall, overweight/obesity (Fig. 2) and pelvic lymph node involvement (Fig. 3) influenced CSS (p = 0.045 and p = 0.003, respectively) in the univariate analysis. Obesity (n = 17) alone also tended to influence the CSS (p = 0.141). There was no significant effect of ICR (n = 23) boost on CSS (p = 0.522). High risk HPV subtypes (16 and 18) did not affect the CSS (p = 0.868). Multivariate analysis (Table 3) showed that pelvic lymph node metastasis was an independent prognostic factor for CSS (p = 0.03).
Discussion and Conclusion
The results of our study show the detrimental effects of overweight or obesity on survival in cervical cancer patients treated with surgery and RT. Survival was related to BMI in cervical cancer. This result reflects the nature of cervical cancer as a metabolic disease.
There are some possible explanations for why BMI can influence the outcome of cervical cancer. Although HPV is the main cause of cervical cancer, PI3K/Akt pathway, has an important role in cancer development [16,17]. Cervical cancer frequently showed activated PI3K pathway. Moreover, PI3K-Akt-mTOR signals amplified by HPV oncogenes E5/E6/E7 activation [18]. This PI3K-Akt-mTOR pathway is important not only in cancer progression but also in cell metabolism. According to Yuan et al. [19], Leptin can increase the proliferation of cervical cancer cells. They argued that Leptin can be involved in the progression of cervical cancer by activation of c-myc and bcl-2 pathway. Also, Leptin receptor stimulation could activate the PI3K-Akt pathway. Moreover, Statins are known to have anti-inflammatory and vascular endothelial protection properties after RT [20]. In other words, lipid lowering drugs can improve the RT outcomes.
During cancer diagnosis, obese patients could have a lower detection rate in Pap smear tests than normal weight patients, because of the difficulty in proper sampling [21]. During treatment, the rates of complete resection or extent of lymphadenectomy in overweight or obese patients might be lower than those in normal weight patients, because of the difficulty of surgical approach [22]. Furthermore, body volume could affect the radiation dose-distribution during RT. The possibility of set-up uncertainty might increase in overweight or obese patients.
Several studies which validate the detrimental effects of overweight or obesity in cervical cancer patients have been reported [10,13,23]. A recent meta-analysis showed that higher BMI was clinically related with cervical cancer risk [10]. Clark et al. [13] also showed that excess body mass index (BMI ≥ 25 kg/m2) was associated with worse survival in cervical cancer patients.
Our study also showed that the importance of body weight in prognosis existed in cervical cancer patients who underwent surgery and RT. Though the standard of overweight/obesity is different to Western standard, BMI can be an important prognostic factor for Asian cervical cancer patients. In this study, the cut-off value of BMI that determined survival was 23 kg/m2 (overweight). The standard of BMI for overweight, according to the World Health Organization (WHO) criteria, is lower in Korea than in Western countries (≥23 kg/m2 vs. ≥25 kg/m2).
Further evaluation is needed to delineate the precise mechanism of the detrimental effects of overweight or obesity on the prognosis of cervical cancer. The pattern of failure might be different in overweight or obese patients than in normal weight patients. In this study, the rate of regional lymph node failure in overweight or obese patients was slightly higher than in normal weight patients, although there was no statistical difference between the two values. Overweight or obese patients might be more easily exposed to regional lymph nodal failures.
There is a need to find effective strategies for early detection or prevention of cervical cancer relapses that are related to excess body weight in patients. The prognostic effects of physical activity and lifestyle change should be more evaluated in the next level studies.
In this study, regional lymph nodal recurrence rate tended to be higher in patients with overweight/obesity. Moreover, pelvic lymph node metastases were related to survival rates after treatment. Therefore, intensity-modulated RT can be used for pelvic lymph nodal irradiation, in order to enable appropriate radiation dose escalation, as this is closely related to increased local control. In addition, more attention should be paid to overweight and obese cancer patients, to find evidence of cancer recurrence in the follow-up periods after treatment. For early detection of recurrence, reducing the follow-up period for overweight or obese patients can be a good strategy.
Limitations of this study should be considered. The number of patients studied was limited to only 70 and this study was based on data from a single institution. Especially, the number of obesity patients was only 17. Thus, it was difficult to get statistically relevant results in this analysis. Moreover, this study was confined to patients who received surgery and RT. Therefore, the association between BMI and cancer progression in patients who underwent RT without surgery was difficult to estimate based on the current study results. More studies are needed to identify the clinical effects of weight reduction in overweight or obese cancer patients, specifically with respect to cancer progression and survival. The discrepancy of detrimental effects of overweight/obesity in treatment failure and survival outcomes should be more evaluated.
In conclusion, overweight or obese cervical cancer patients showed poor survival outcome compared to normal weight or underweight patients. The importance of body weight in the prognosis of cervical cancer after treatment should not be ignored. Careful observation is needed for overweight or obese cervical cancer patients. Maintaining normal body weight or underweight seems to improve cervical cancer survival outcome. Recommendation of lifestyle modifications can be considered an important aspect of clinical management for cervical cancer patients who have undergone surgery and RT.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.