Comparison between audio-only and audiovisual biofeedback for regulating patients' respiration during four-dimensional radiotherapy
Article information
Abstract
Purpose
To compare audio-only biofeedback to conventional audiovisual biofeedback for regulating patients' respiration during four-dimensional radiotherapy, limiting damage to healthy surrounding tissues caused by organ movement.
Materials and Methods
Six healthy volunteers were assisted by audiovisual or audio-only biofeedback systems to regulate their respirations. Volunteers breathed through a mask developed for this study by following computer-generated guiding curves displayed on a screen, combined with instructional sounds. They then performed breathing following instructional sounds only. The guiding signals and the volunteers' respiratory signals were logged at 20 samples per second.
Results
The standard deviations between the guiding and respiratory curves for the audiovisual and audio-only biofeedback systems were 21.55% and 23.19%, respectively; the average correlation coefficients were 0.9778 and 0.9756, respectively. The regularities between audiovisual and audio-only biofeedback for six volunteers' respirations were same statistically from the paired t-test.
Conclusion
The difference between the audiovisual and audio-only biofeedback methods was not significant. Audio-only biofeedback has many advantages, as patients do not require a mask and can quickly adapt to this method in the clinic.
Introduction
Normal tissue damage during lung cancer radiotherapy is generally due to large treatment margins. Organ motion due to respiration requires that large margins be included in the planning target volume for adequate dose coverage in the chest and abdomen [1]. There are a few techniques available to minimize respiratory induced organ motion, such as active breathing control that holds patients' breaths spontaneously [23456], respiration gated radiation therapy [78], and adaptation of radiation fields to a moving target by continuously utilizing information on the location of the internal target by direct or indirect monitoring [9101112]. To administer respiration adaptive radiation therapy effectively, it is essential to regulate patients' respiration, and many researchers have explored this concept [13141516]. We previously explored regulating respiration using audiovisual biofeedback, which regenerated patients' actual breath signals iteratively [17]. The audiovisual biofeedback was effective for regulating patients' respiration; however, a screen had to be installed and the patient had to wear the goggle for obtaining visual feedback. Adapting the patients to the audiovisual biofeedback devices to the patients needed at least 10 minutes in clinics. Some busy departments may have difficulties in setting up such devices.
Conversely, the audio-only feedback method does not require the installation of screen or wearing the goggle for video guidance in the treatment room; patients merely listen to a sound emitted from a speaker fixed to the wall or ceiling.
The purpose of this study was to compare the effectiveness of audiovisual versus audio-only biofeedback, and to see whether audio-only biofeedback is a practical alternative for regulating patients' respiration during four-dimensional radiation therapy.
Materials and Methods
1. Respiration monitoring system
The respiration monitoring mask (ReMM) was previously developed with a chromel-alumel (K-type) thermocouple to measure respiration while indirectly monitoring tumor motion [1819]. The thermocouple measures temperature changes at the center of the air stream from the nose and mouth in a commercial dustproof mask (N7000; Woori Tech Co., Seongnam, Korea) (Fig. 1). The cool air from outside the mask flows into the mask when the patient inhales, and the mask is filled with warm air from a patient's lung when he/she exhales. In this manner, the thermocouple measures the change of temperature in the mask as the patient breathes. The end of the thermocouple was connected to the operational amplifier chip (AD597AH; Analog Devices, Norwood, MA, USA). The thermocouple signals were digitized in real time with a data acquisition card (DAQ 6024E; National Instruments, Austin, TX, USA). Continuous temperature readings corresponding to the respiration were analyzed and stored at 100 samples per second. The program for acquiring and analyzing respiratory signals was built using LabVIEW 7.0 (National Instruments).
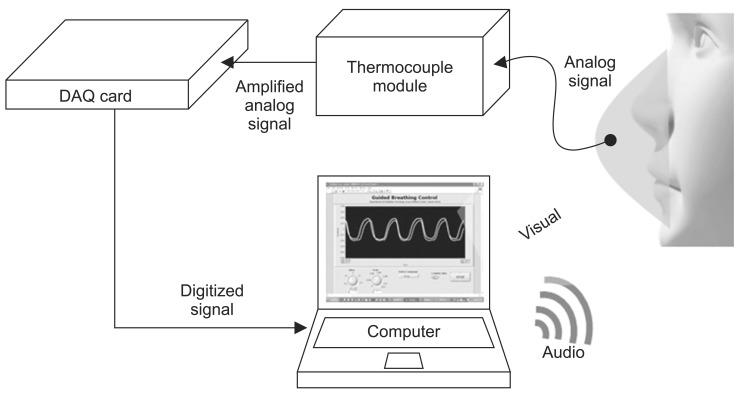
Schematic diagram of the Audiovisual Guided Breath System. The respiratory signal from the respiration monitoring mask is amplified by the thermocouple module and digitized by the analog-to-digital converter. The computer generates the guiding signal and acquires the respiratory signal. DAQ, data acquisition.
A system that regulates a subject's respiration consists of a ReMM, a thermocouple module, the analog-to-digital converter card, one screen each for the operator and the patient (although only one was used in this study for the volunteers), a speaker, and a computer.
2. Patients' respiration regulating system
In order to enable the patients to breathe regularly, we developed the audiovisual biofeedback system using the ReMM in a previous study [17]. The setup of this system is the same as shown in Fig. 1. The program was optimized to allow audiovisual feedback. Two curves are displayed on the screen: one indicates the patient's current respiration pattern and the other is a guiding signal, which represents a single respiration cycle that was acquired by monitoring each volunteer's regular respiration with the ReMM and was then continuously reproduced (Fig. 2). The guiding sound was a beep; alternatively, Korean and English language instruction voices were available (Fig. 3). Audio biofeedback was for auxiliary guidance in case the patient looked away from the screen displaying the guiding curve for any reason.
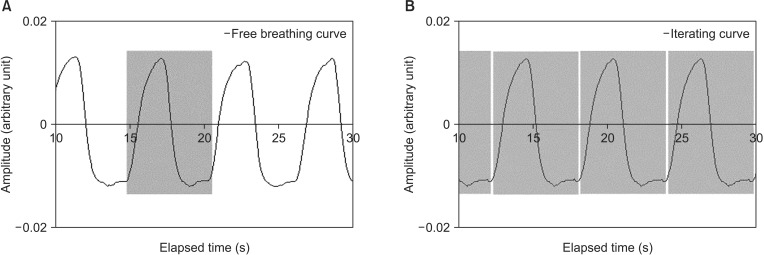
Generating the guiding curve. (A) Free respiration: a single curve cycle is extracted from the actual respiration during normal respiration for each volunteer. (B) Guiding curve: the single extracted curve from panel A was then iterated.
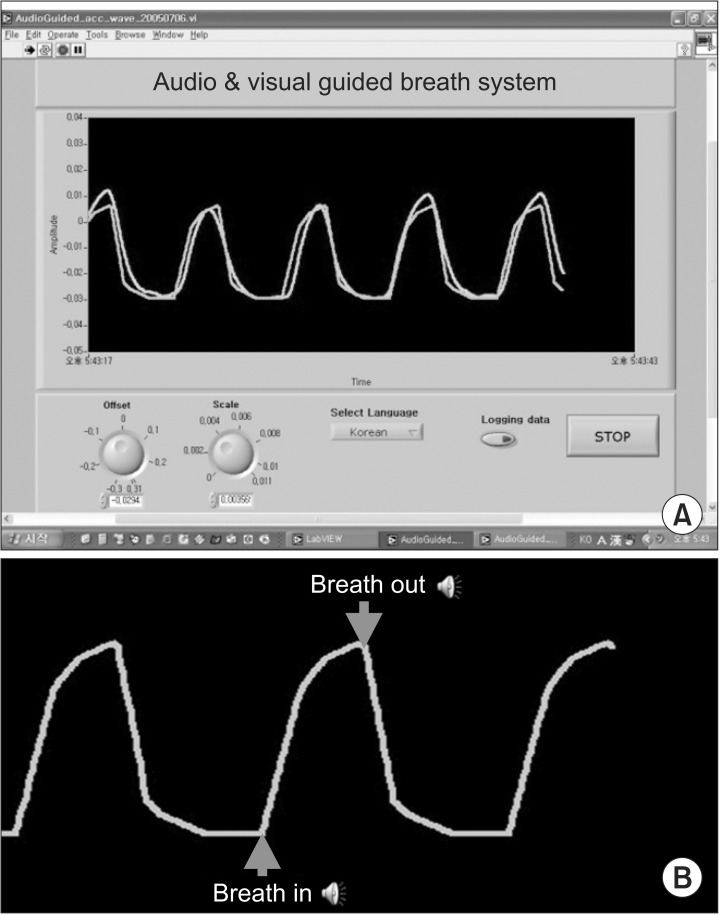
(A) Audiovisual assistance: the gray curve represents the guiding curve while the green curve represents the respiratory curve. (B) Audio assistance: this was programmed to sound out the words "breath out" when the curve on the peak, and "breath in" when on the trough. The sounds were based on the guiding curve. A preferred language (Korean or English) could be selected; otherwise, a beep would sound instead.
3. Audiovisual versus audio-only biofeedback
All volunteers were instructed to breathe following their own guiding curve, and to control their breath by watching the screen and listening to the audio instruction. Six healthy volunteers are enrolled to test this system. After a 5-minute instruction session, volunteers breathed through the ReMM by following the guiding curves and sounds simultaneously; in the subsequent session, they followed only the sound guidance based on the guiding curve. The guiding signal and the volunteers' respiration signals were logged at 20 samples per second. Volunteers' respirations with both biofeedback assistances were logged using the ReMM for 60 seconds, respectively. Then we calculated standard deviation of amplitude in percent (amplitude of guiding curve is 100%) and correlation coefficient for volunteers' respiration signal comparing to its guiding curve. The correlation coefficient takes into account shape differences of the curves and the standard deviation is for evaluating the difference of amplitudes.
Results
The system responded dynamically to the volunteers' respiration signals, which were displayed directly on the screen. The delay time was of the order of a few milliseconds, which is negligible in clinics. Volunteers followed the guided curves effortlessly, as the system continuously generates respiration cycle representative of their actual respiration patterns. The volunteers were more comfortable with the audio-only biofeedback than with the audiovisual biofeedback procedure because they did not require the screen and goggle.
Table 1 shows the correlation coefficient and the standard deviation of amplitudes between the reference signal (the guidance curves) and the volunteers' respiration curves for both audiovisual and audio-only biofeedback. The average correlation coefficients between the guidance and the respiration curves for volunteers assisted by audiovisual and audio-only biofeedback systems were estimated as 0.9778 and 0.9756, respectively. The standard deviation between the guiding curves and the respiration curves were 21.55% and 23.19% for the audiovisual and the audio-only biofeedback, respectively. The significance levels of differences between guiding and respiration curves for audiovisual and audio-only biofeedback were evaluated. The regularities of both biofeedback were not different statistically with p-values of 0.335 and 0.837 for standard deviation and correlation coefficient, respectively, at the 5% significant level from the paired t-test. Fig. 4 shows the first volunteer's respiration curves. Fig. 4A and B show the respiration data obtained by audio-only biofeedback assistance, whereas Fig. 4C and D show respiration data obtained by audiovisual biofeedback assistance. The audiovisual biofeedback was slightly superior to the audio-only biofeedback according to our data.
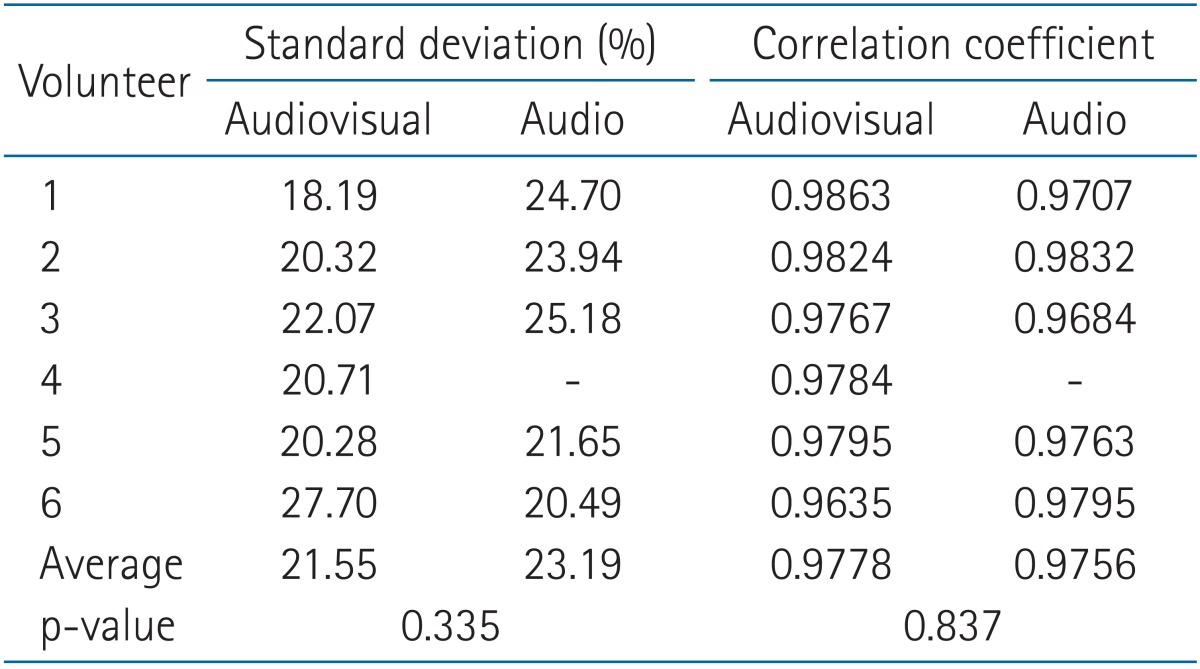
Relationship between the guiding curve extracted from the actual respirations of six volunteers and the respiration signal: audiovisual feedback was slightly superior to audio-only biofeedback
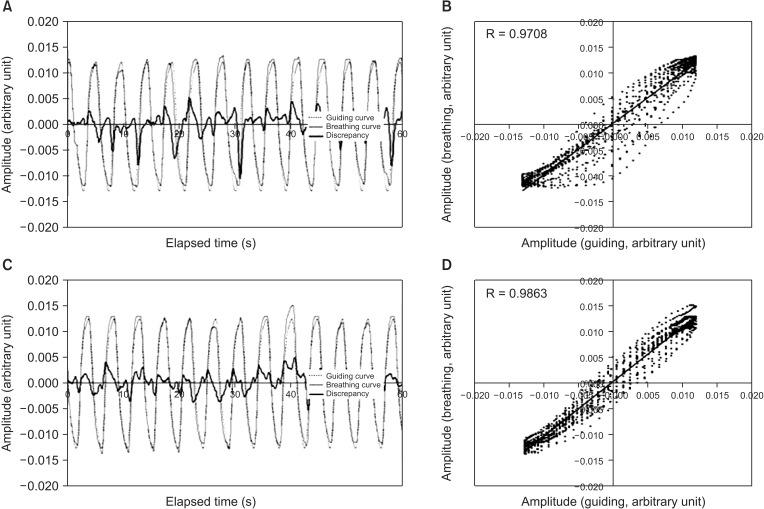
Comparison between guiding curves and respiration curves for volunteer 1 (A) the discrepancy between the audio-only guiding curve and respiration curve. (B) The correlation between the two sets of curves in panel A. (C) The discrepancy between the audiovisual guiding curve and respiration curve. (D) The correlation between the two curves in panel C.
Discussion and Conclusion
Monitoring fluoroscopic images is the most direct method to measure the respiratory induced organ motion. However unnecessary radiation doses can be delivered to patients [9202122]. The Real-time Position Management (RPM) which detect skin motion using infrared reflectors is a commercialized tool for monitoring organ motion indirectly. A spirometer can also be used to measure respiration; however, there is a problem of baseline-level drift of respiratory signal. These indirect methods require correlation with the target motion. Kubo and Hill [7] showed that the temperature sensor is reproducible and accurate. The temperature sensor has many advantages for monitoring target motion for 4D radiotherapy. The ReMM made with thermocouple showed a strong correlation with respiratory induced organ motion in the previous study, indicating that organ motion could be reliably determined from the information obtained via ReMM [19]. The respiration regulating system developed in the previous study used the audiovisual biofeedback method [17]. Patients were comfortable with the guiding curves, since the system continuously generates a respiration cycle based on their own.
However, audio-only biofeedback has many advantages over audiovisual biofeedback, particularly in overburdened clinics. Patients do not require the screen and goggle and can adapt quickly to the system. In this study, we aimed to show that audio-only biofeedback is also practical, especially as the difference between audio-only versus audiovisual biofeedback was not significant. The limitation of this study is the number of volunteers and the fourth volunteer did not perform audio-only biofeedback assistance. The sequence of measurements of audiovisual and audio-only biofeedback could result in bias in overestimating regularity of audio-only biofeedback assistance. In the future we need to evaluate this study with enough volunteers and alternative sequences. The respiration regulation is not mandatory but it has been reported that the more regular respiration, the more effective 4D radiotherapy such as gated or breath hold radiotherapy [1314151617]. This study showed that audio-only biofeedback was simple and practical method to regulate respiration.
Acknowledgments
This research was supported by Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Education, Science and Technology (2010-0013701 and 2013R1A1A2012013).
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.