Treatment outcome of conservative surgery plus postoperative radiotherapy for extremity soft tissue sarcoma
Article information
Abstract
Purpose
To evaluate the treatment outcome and prognostic factor of postoperative radiotherapy for extremity soft tissue sarcoma (STS).
Materials and Methods
Forty three patients with extremity STS were treated with conservative surgery and postoperative radiotherapy from January 1981 to December 2010 at Korea University Medical Center. Median total 60 Gy (range, 50 to 74.4 Gy) of radiation was delivered and 7 patients were treated with chemotherapy.
Results
The median follow-up period was 70 months (range, 5 to 302 months). Twelve patients (27.9%) sustained relapse of their disease. Local recurrence occurred in 3 patients (7.0%) and distant metastases developed in 10 patients (23.3%). The 5-year overall survival (OS) was 69.2% and disease free survival was 67.9%. The 5-year local relapse-free survival was 90.7% and distant relapse-free survival was 73.3%. On univariate analysis, no significant prognostic factors were associated with development of local recurrence. Histologic grade (p = 0.005) and stage (p = 0.02) influenced the development of distant metastases. Histologic grade was unique significant prognostic factor for the OS on univariate and multivariate analysis. Severe acute treatment-related complications, Common Terminology Criteria for Adverse Events (CTCAE) grade 3 or 4, developed in 6 patients (14.0%) and severe late complications in 2 patients (4.7%).
Conclusion
Conservative surgery with postoperative radiotherapy achieved a satisfactory rate of local control with acceptable complication rate in extremity STS. Most failures were distant metastases that correlate with tumor grade and stage. The majority of local recurrences developed within the field. Selective dose escalation of radiotherapy or development of effective systemic treatment might be considered.
Introduction
Soft tissue sarcoma (STS) is a rare tumor accounts for less than 1% of all newly diagnosed malignant diseases and extremity is the most common site of origin [1]. STS extensively invades surrounding soft tissue, so local recurrence rates are as high as 30% to 50% with local excision only [2]. Radical excision and amputation were used to improve local control and multimodality approach with conservative surgery plus postoperative radiotherapy is being used since 1970s for the purpose of preserving limb function and local control [2].
STS has a tendency to metastasize early and approximately one-half of the patients died of their disease [3]. The relationship between local control and survival has been under controversy, but Lewis et al. [4] suggested that there is a strong association of local recurrence with development of subsequent metastases and tumor mortality. Prognostic factors for local control and disease free survival are known to be histologic grade, tumor size and depth. Histologic grade is the most important prognostic factor for overall survival and predicting metastases [3].
In this article, we retrospectively analyzed the treatment outcomes and prognostic factors of localized extremity STS patients treated with conservative surgery plus radiotherapy.
Materials and Methods
1. Patient and tumor characteristics
Between January 1981 and December 2010, 43 adult patients (>16 years) with non-recurrent STS of extremities were treated with conservative surgery and postoperative radiotherapy at Korea University Medical Center (KUMC). Patients who had distant metastases, who had local recurrence at the time of presentation, or who irradiated with doses less than 40 Gy were excluded from this study. The following histologic subtypes were also excluded: Ewing's sarcoma, desmoid tumor and rhabdomyosarcoma [5-8].
Twenty four patients were male and 19 were female. Ages ranged from 20 to 71 years with a median of 44 years. Forty three consecutive patients with STS in whom all visible tumors had been resected underwent radiation therapy with curative (postoperative) intent. Medical records of all patients were available for review.
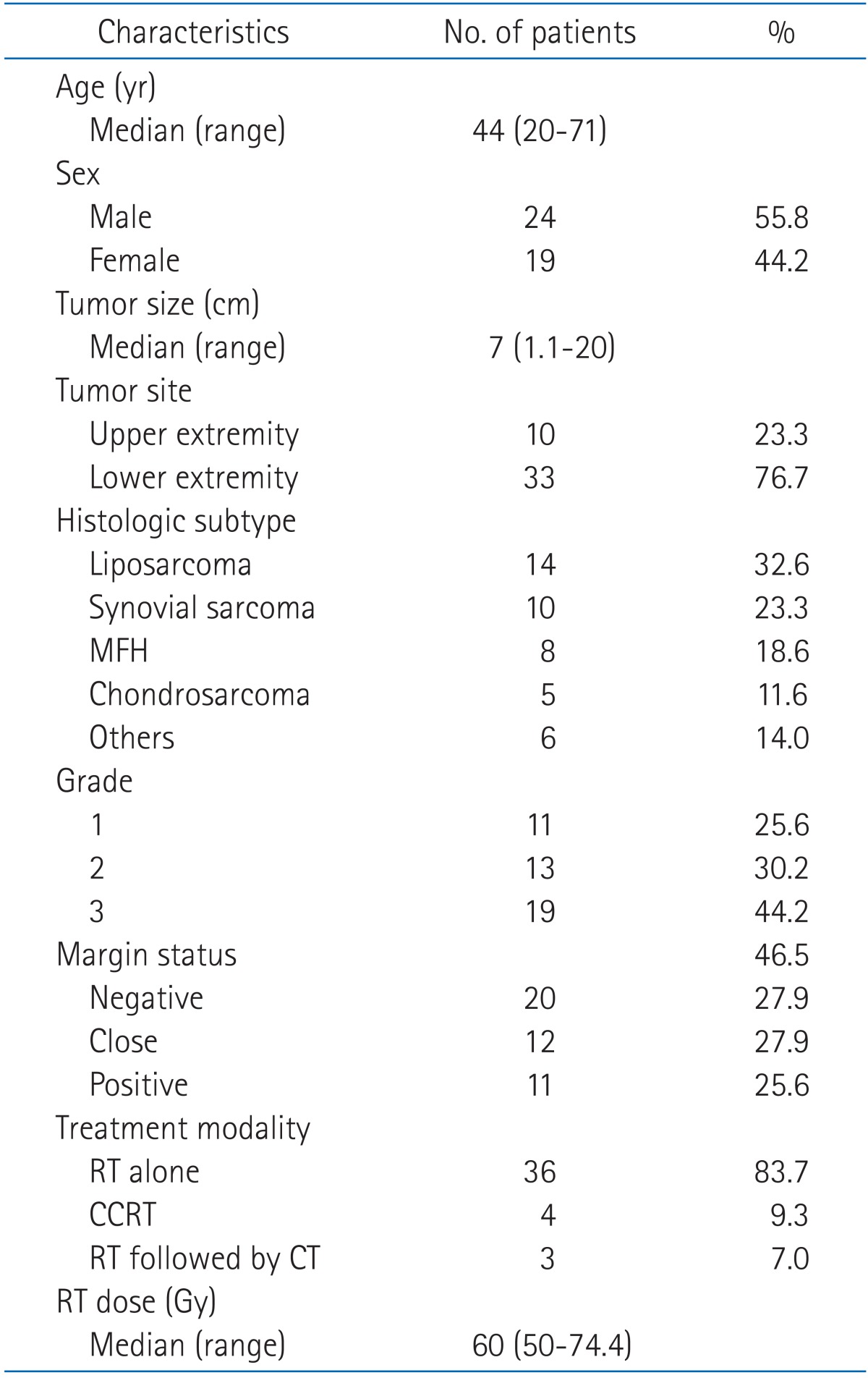
The distribution of lesions by anatomic site was as follows. Ten (23.3%) were in the upper extremity, 2 in the wrist and hand, 4 in the forearm, 1 at the elbow, and 3 in the upper arm and shoulder. Thirty-three (76.7%) were in the lower extremity, 23 in the thigh region, 1 in the knee region, 2 in the lower leg, 3 in ankle and foot, and 4 in the inguinal and gluteal region. Patient characteristics at the time of presentation are outlined in Table 1.
There were 11 patients with positive margins and most common histology was synovial sarcoma (36.4%) followed by malignant fibrous histiocytoma (MFH, 27.3%). Eight of 11 patients were with grade 3, 2 with grade 2 and 1 with grade 1.
2. Treatment
The fundamental treatment strategy for STS at KUMC has been a combination of conservative surgery and postoperative radiotherapy. Treatment characteristics are summarized in Table 1.
1) Surgery
All patients underwent surgery with the intention of a wide resection when possible and the goal was to obtain tumor-free margins of 1-3 cm. When this was not feasible because of adjoining critical structures, an attempt was still made to obtain tumor-free, but closer margins. Expert pathologist determined the histology and assigned a grade based on Fédération Nationale des Centres de Lutte Contre le Cancer (FNCLCC) system [9]. A positive margin was defined as the presence of tumor at the margin of the resected specimen. A close margin was defined as less than 2 cm from resection margin by Rubin et al. [9] and this reviewed individually in our center considering anatomical barrier by specialized pathologist.
2) Radiotherapy
Radiotherapy (RT) was administered with cobalt-60 (ATC C9; Picker Corporation, Cleveland, OH, USA) or mostly 4 megavoltage X-rays by linear accelerator (LINAC, Varian Clinac 600C; Varian Medical Systems, Palo Alto, CA, USA). General indications for RT included pT2 or greater, high grade histology and close or positive margins. Postoperative RT was delivered to median 60 Gy (range, 50 to 74.4 Gy) using one to three beams. The dose per fraction were 1.8 Gy (34.9%) or 2.0 Gy (65.1%) and the median duration of RT was 49 days (range, 35 to 80 days). The median time between surgery and initiation of RT was 21 days. No attempt was made to irradiate the entire muscle compartments or muscle bundles from origin to insertion. The entire circumference of an extremity was never treated and care was taken not to treat more than half of long bones and to spare joints. RT field was designed encompassing the surgical bed/scar plus up to 5 to 6 cm margin. Twenty-five patients were available of initial field-margin status and 0 to 5 cm margin (median, 2 cm) was added from the end of surgical bed/scar, which depends on tumor size, histological grade and tumor site.
3) Chemotherapy
No standard criterion for the administration of chemotherapy existed for patients in this study. Systemic chemotherapy was given to 7 patients (16.3%): 5 patients received adjuvant chemotherapy and 2 patients received both neoadjuvant and adjuvant chemotherapy. The recommendation for the use of chemotherapy was based on the multidisciplinary judgment. Doxorubicin-based chemotherapy was the most frequently used regimen.
3. Follow-up and statistical analysis
Follow-up was done one month after treatment completion, then every 3 months for first 2 years, every 6 months thereafter during 3 years, and then yearly. Times of follow-up were measured from the date of diagnosis. The follow-up time for all patients ranged from 5 to 302 months with median of 70 months. The follow-up data was obtained from RT records and hospital charts. Computed tomography/magnetic resonance imaging or bone scan were performed when patient have symptom or judged to be necessary by clinician. Additional imaging study and biopsy were done when suspected for recurrence. Overall survival, prognostic factors and complication were analyzed retrospectively. Common Terminology Criteria for Adverse Events (CTCAE) v4.0 was used for acute and late complication.
Local recurrence was defined as the first recurrence of the disease at the site of primary tumor, of the same histologic subtype, that occurred more than 3 months after primary therapy. Overall survival (OS) rate was defined as duration from the day of surgery to the date of death or last date for censored observation. Local relapse-free survival (LRFS) or distant relapse-free survival (DRFS) was defined as the duration from the day of surgery to date of each recurrence observed. Relapse or death from any cause was considered as disease-free survival (DFS) event. Deaths that were confirmed to be caused by disease were treated as an end point for disease-specific survival (DSS), while other deaths were treated as censored observations.
Statistical analysis was performed using SPSS ver. 19.0 (SPSS Inc., Chicago, IL, USA). LRFS, DRFS, OS, DFS, DSS and the probability of complications were calculated using the Kaplan-Meier method and compared using the log-rank test. Multivariate analysis was performed using Cox proportional hazards model. In all statistical analyses, a p-value less than 0.05 considered significant.
Results
1. Patterns of failure
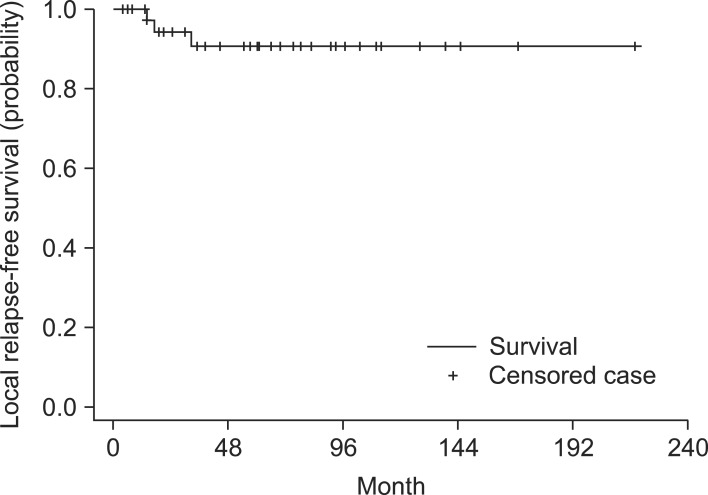
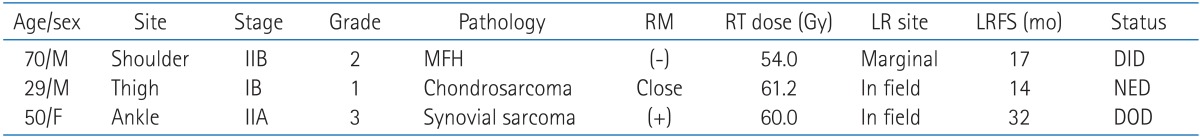
Twelve patients (27.9%) sustained relapse of their disease. Local recurrence occurred in 3 patients (7.0%). The time to local recurrence varied from 14 to 32 months (median, 17 months). All local recurrences occurred within 3 years. The actuarial LRFS at 2 and 5 years were 94.2% and 90.7%, respectively (Fig. 1). One patient with negative margin had received 54 Gy and demonstrating recurrence on the margin of the field. Two patients received at least 60 Gy and have been divided into one with close and one with positive margin (Table 2). Both patients recurred within the field. For salvage treatment of local recurrence, two patients underwent surgical resection and one patient had re-irradiation. After salvage treatment, one patient alive 34 months after recurrence without evidence of disease and two died: one died of recurrent disease and the other died of intercurrent disease.
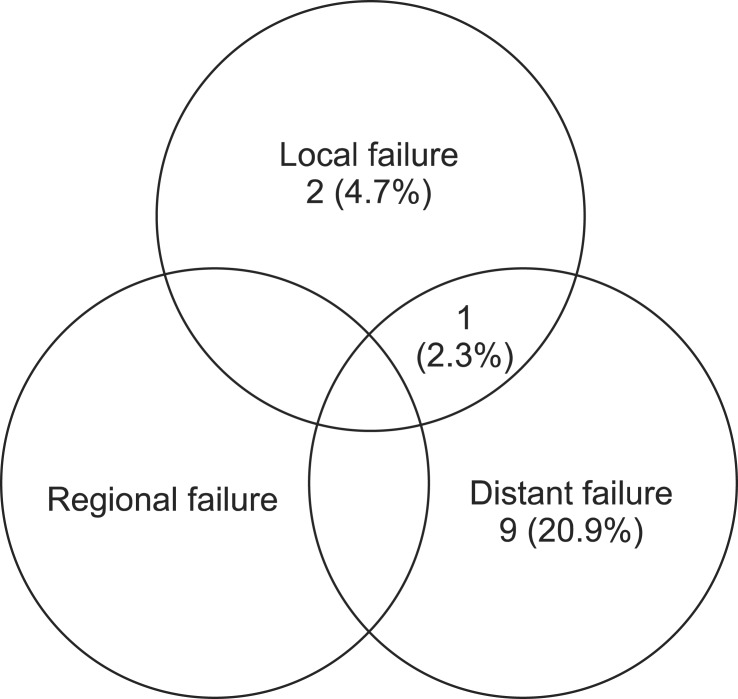
No regional lymph node metastases developed. Hematogenous metastases developed in 10 patients (23.3%) and those were the first site of disease relapse in 9 (Fig. 2). The actuarial DRFS rates at 2 and 5 years were 86.4% and 73.3%, respectively. The most common site for distant metastasis was lung (70%) followed by bone (20%) and retroperitoneum (10%). And for the treatment of distant recurrence, 4 patients had RT, 4 received chemotherapy, and 2 patients underwent metastasectomy and chemotherapy.
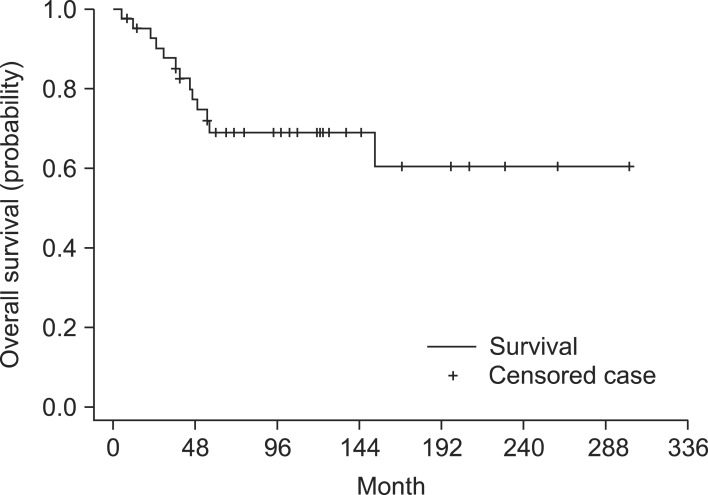
2. Survival rates
The OS curves for all 43 patients are shown in Fig. 3. Survival rates at 2, 5 years were 92.7% and 69.2%, respectively. The mean survival time was 207 months (95% confidence interval [CI], 164 to 250). DFS at 2, 5 years were 80.8% and 67.9% with mean times of 148 months (95% CI, 115 to 180). DSS at 2, 5 years were 92.7% and 74.0% with mean times of 218 months (95% CI, 175 to 261).
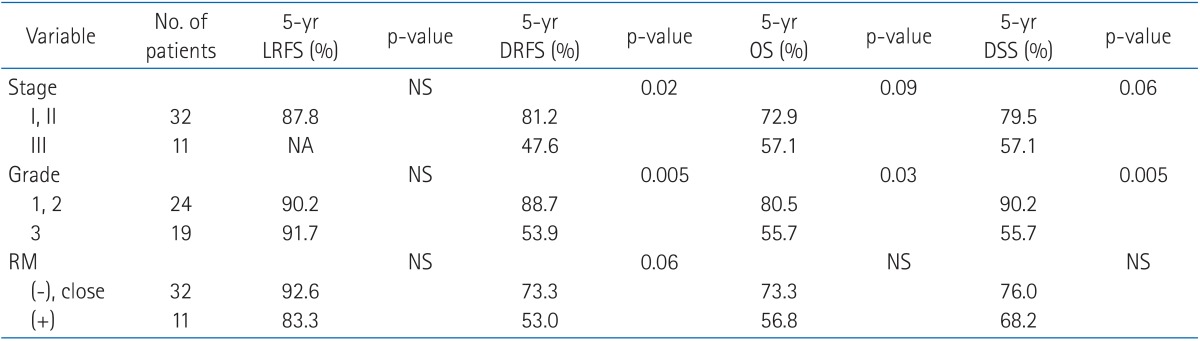
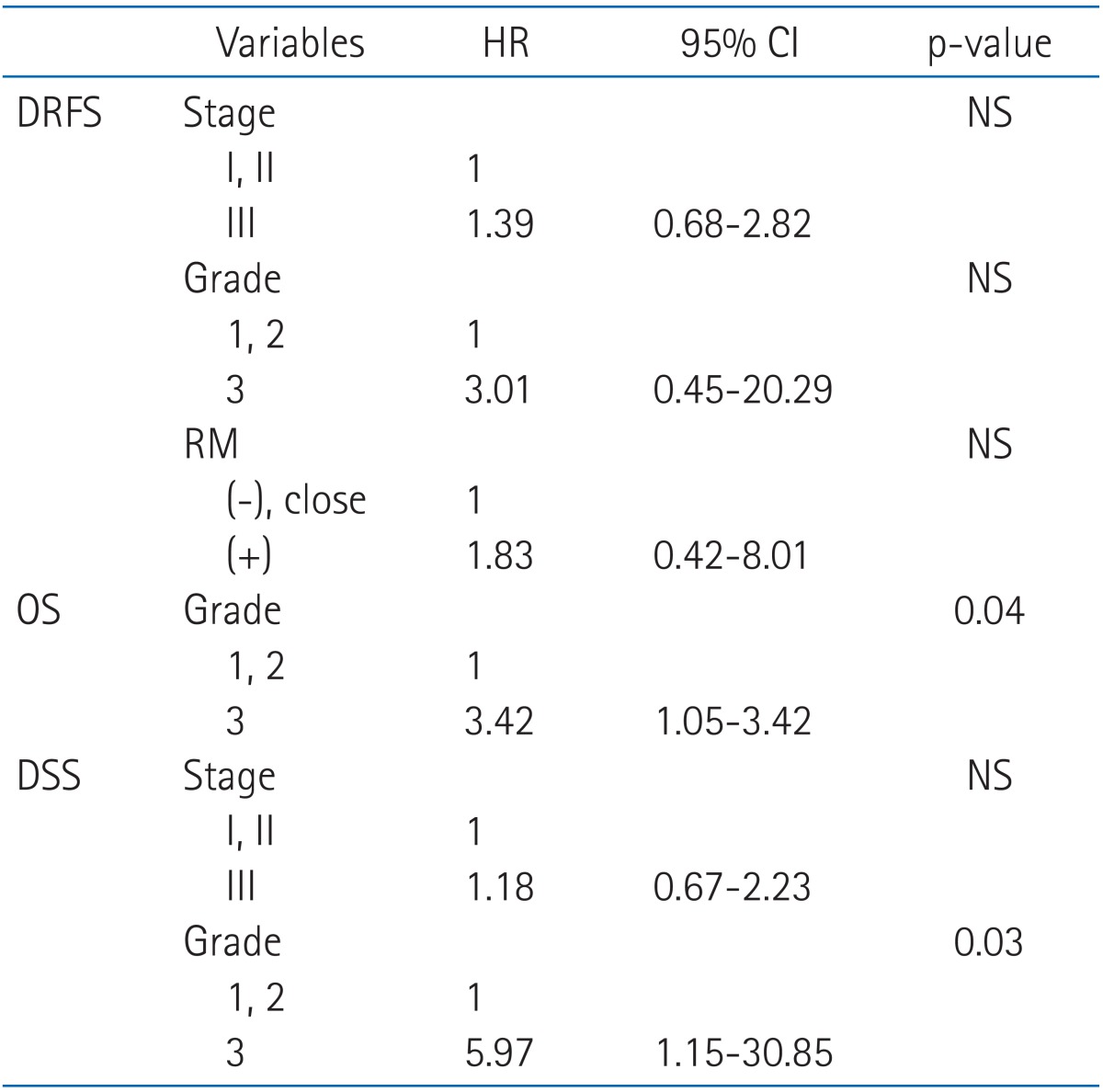
3. Prognostic factors
On univariate analysis, grade did not have a significant impact on local control, but did influence on DRFS (p = 0.005), DSS (p = 0.005) and OS (p = 0.03). No significant prognostic factors were associated with development of local recurrence. American Joint Committee on Cancer (AJCC) stage (p = 0.02) and grade (p = 0.005) influenced the development of distant metastases in the univariate analysis. A trend toward higher risk of distant metastases was also noted among patients with positive margins (p = 0.06) (Table 3). On multivariate analysis, grade had only a significant impact on OS (p = 0.04) and DSS (p = 0.03) (Table 4).
4. Complications
Acute radiation-related complications, grade 3 or 4, according to CTCAE v4.0 developed in 6 patients (14.0%). Four patients had skin desquamation (9.3%), one patient had pruritus (2.3%) and one patient had skin ulceration (2.3%). The incidence of complications was significantly higher among the patients receiving chemotherapy compared with those not receiving chemotherapy (42.9%, 8.3%, respectively; p = 0.02). All three patients received chemotherapy concurrently with radiotherapy. Neither radiation dose nor irradiated field size correlated with acute complication risk.
Severe late radiation-related complication, grade 3 or 4, developed in 2 patients (4.7%): one lymphedema and one skin ulceration. These began at 4 and 62 months after radiotherapy (Table 5). Irradiated dose of the two patients was 61.2 Gy and 66.6 Gy, respectively.
Discussion and Conclusion
The aim of the treatment in STS is to achieve local control and cure while ensuring organ preservation and limb function. Conservative surgery and postoperative radiotherapy are the preferred treatment in order to avoid amputation and this conservative approach offers high local control similar to those reported with amputation [3,10-13]. Whether improved local control translates to improved survival remains controversial [11,13]. In Lewis's analysis local recurrence has strong association with tumor-related mortality [4]. However, this may be because locally recurrent tumors are biologically more aggressive rather than a causal relationship [14].
Several prognostic factors for local recurrence have been reported, and these were included in our analyses. High grade, distal extremities and positive microscopic margin have been analyzed as prognostic factors influencing local recurrence [3]. Specific histologic types have been associated with high risk of local recurrence, especially in MFH [15]. In our study, we were not able to find any correlation between these factors and local recurrence and there was no correlation between treatment characteristics (radiation dose, field margin, and use of chemotherapy) and local recurrence. However, the patients who underwent RT were more likely to have had deep location, high grade tumors excised with a close or positive margin. In our analysis, histology of 3 recurrent patients was MFH, chondrosarcoma and synovial sarcoma. The lack of associated factor of local recurrence may be due to the small number of patients involved in this study, further studies are needed.
In our series the 5-year actuarial local control rate was 90.7% and it was comparable to other reported studies which achieve 5-year local control rates of 85% to 90% [14]. Three patients had local recurrence and two had recurred within the field, one in the margin of the field. Our result was comparable to other studies previously reported that the majority of the local recurrence was found within the field [14,16]. Cleator et al. [14] demonstrated 68% of local recurrence was within the field, 16% were out of the field, and 16% were on the margin of the field. In Dickie et al. [16]'s analysis of 768 patients 49 cases recurred within the field (6.4% overall), 9 were out of the field (1.1% overall), and 2 were on the margin of the field (0.3% overall).
Initial field margin of at least 5 cm around the tumor bed/scar are known to achieve superior local control in the postoperative radiotherapy [13]. But field margin needed to include potential microscopic disease is poorly defined [3]. A margin of only 2 cm around the tumor was added for brachytherapy and actuarial local control rate for high grade tumor are about a 90% [11] and this was comparable local control with wide field margin added for external beam radiotherapy. Afterloading catheters were placed intraoperatively in the tumor bed for brachytherapy and this made more accurate targeting thereby limited volume was irradiated and did not introduce long term functional morbidity [11]. Our initial filed margin was 0 to 5 cm (median, 2 cm) to the tumor bed including scar and this was applied individually according to surgical extent. However with this limited margin a 91% of local control was achieved. Possible explanation may be that the surgical technique may have a considerable impact on the degree of dissemination of tumor cells [3] or may be that only limited margin is needed to control disease when accurate targeting was done. And reduction of normal tissue irradiation with limited planning target volume margin in an evidence-based and quantitative manner should not increase the risk of local recurrence [16]. To reduce normal tissue irradiation, traditional 5 cm longitudinal margin from the end of tumor bed may be shortened. Further studies are needed to define optimal margin for radiotherapy.
In general, the postoperative radiotherapy (PORT) dose used in most centers is 50 Gy (range, 40 to 50 Gy) and boost of at least 10 Gy is given to high risk areas [3]. Although adequate dose in PORT has not been established, improved local control rate are associated with higher dose above 60 Gy [3,10,17]. In the literature, dose was escalated up to 70 Gy for patient with residual tumor or positive resection margin. In our analysis, almost local recurrence occur within the field, so it seems to be dose escalation to tumor bed is required for tumor control. Dose escalation might improve local control when target volume can be exactly defined and covered. But, severe complications are accompanied with higher dose above 63 Gy [13]. Thus selective dose escalation of radiotherapy might be considered for high risk patients and reappraisal of adequate dose to low risk patients might be considered. Patient with negative margins can be treated less than 60 Gy without compromising local control and fewer complications [13]. Tailored treatment might be needed according to risk group and whether dose escalation can be translated into improved outcome will be assessed after a longer follow up period.
In our series, the 5-year DRFS and OS are 73.4% and 69.2%, respectively and it was comparable to other reported studies [2,15,18]. The well-established prognostic factors for tumor related death from STS are histological grade, tumor size and age [3]. Our multivariate analysis also demonstrated higher OS and DSS rate for low grade tumor. And histologic subtype was not a significant determinant of outcome in our series. Univariate analysis revealed that histologic grade, AJCC stage and resection margin status were independently correlates with development of distant metastasis. But these were not significant determinants on multivariate analysis. STS have a tendency to metastasis early and the poor survival of such patients has led to a search for systemic treatments that might be applied early in the course of the disease [2]. Development of effective systemic treatment might be considered.
The 14% incidence of acute complications reported in our series is similar to that reported by other authors. As for acute side effects, skin desquamation was occurred in 4 patients, 1 patient suffered from pruritus and 1 patient had skin ulceration. Our data suggests patient with chemotherapy may be associated with an increased risk of complications than patient without chemotherapy. The RT treatment volume defined for STS multimodality management has been predictive of late RT effects such as fibrosis, edema, and joint stiffness and a reduction of normal tissue irradiation may translate into a decrease in such radiation-related toxicities [16]. Modern treatment techniques, such as intensity-modulated radiotherapy (IMRT), have facilitated highly conformal targeted approaches with a reduction in the overall treatment volume exposed to higher doses to reduce complication. However, this reduction may potentially expose the patient to an increased risk of local recurrence (LR).
In conclusion, conservative surgery with postoperative radiotherapy achieves a satisfactory rate of local control with acceptable complication rate in extremity STS. However, this disease has a high distant metastatic propensity that correlates with tumor grade and stage. Tumor grade was the most important factor for overall survival and there was no significant factor associated with local recurrence. The majority of the LRs developed in the irradiation field regardless of surgical margin status or total accumulative RT dose. And this may indicating that the incidence of LR is not predominately caused by aberrations in RT dose or target volume coverage but by biologic behavior of tumor. Development of effective new systemic treatment for this disease is an urgent priority for tumor with high grade or high stage to reduce distant metastasis. And the newly developing radiation technologies such as IMRT and image-guide radiotherapy have a beneficial effect in dose escalation and sparing normal tissue.
Notes
No potential conflict of interest relevant to this article was reported.